**The Transition from Patient-Focused Care to Corporate-Influenced Healthcare**
In the past few decades, the shift of healthcare from a patient-focused approach to a profit-centered sector has been evident. The political discussions regarding the Affordable Care Act (ACA) frequently overlook the fundamental problems that increase premiums and limit access for the average American.
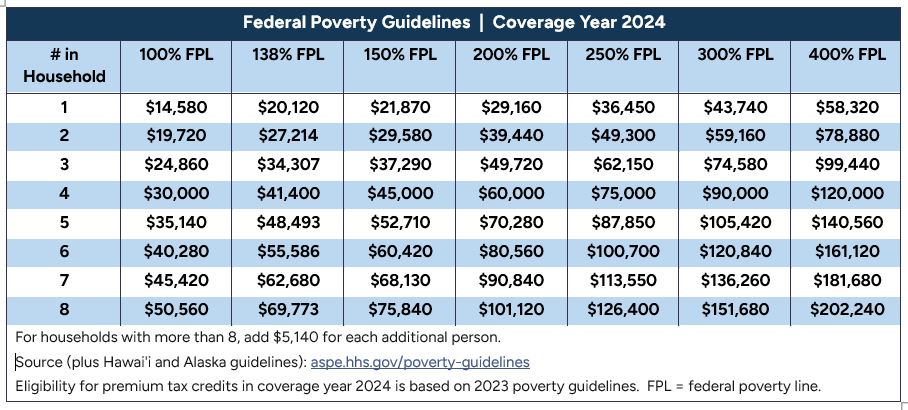
A significant oversimplification in current discussions is the notion that if Republicans manage to allow ACA tax credits to lapse, insurance prices will rise uncontrollably. Initially, the ACA offered premium tax credits for individuals earning up to 400% of the federal poverty level (FPL). A temporary extension was introduced with the 2021 American Rescue Plan, expanding subsidies to 700% of the FPL, thereby temporarily assisting numerous upper-middle-income families. The impending expiration concerns this particular extension, not the essential ACA provisions.
Insurance prices are undeniably increasing, but the main drivers are not widely communicated. It’s the commercialization of the ACA’s structural design by corporate entities that propels costs higher. The ACA’s medical loss ratio rule and other regulations encourage greater spending rather than enhancing patient outcomes, creating a scenario where healthcare costs uncontrollably escalate.
In addition, the consolidation of both hospitals and insurers has diminished competition. Major health systems, after acquiring many physician practices, possess considerable power to set prices. As they close community hospitals and enforce patient dependence on their networks, routine office visits now incur “facility fees,” raising previously manageable expenses.
The reduction of independent physicians—once champions of reliable, accountable care—can be linked to governmental reimbursement tactics biased toward benefiting large medical entities. Each merger and acquisition further infringes upon patient autonomy.
Moreover, several nonprofit hospital systems leverage their tax exemptions, exhibiting behaviors akin to aggressive for-profit organizations—reporting substantial surpluses, investing in high-end properties, and pursuing collections from financially strained patients while claiming to serve public welfare.
Consider the 340B drug discount program; it was originally designed as a benefit for underserved patients. Now, it operates as a revenue source for hospitals purchasing medications at discounted prices intended for low-income patients, reselling them at retail prices, and pocketing the resultant profits.
Adding to the complexity is the unyielding rise in drug prices, particularly for specialty biologics. Pharmacy Benefit Managers (PBMs) distort the market by adjusting rebates and formulary structures to benefit corporate profits rather than reducing patient costs.
Restoring affordability and integrity in American healthcare requires moving beyond partisan rhetoric. The entrenchment of incentives that prioritize corporate profits over patient well-being must be confronted directly. Without addressing these fundamental concerns, changes in subsidies alone cannot alleviate the systemic challenges facing healthcare.
*Andrew Murphy is an allergy-immunology physician.*