I once thought that being an effective physician required generosity, adaptability, and a willingness to overlook regulations for the sake of a patient. That perspective has changed.
The insight originated from a young patient who entered my traditional Chinese medicine (TCM) clinic one day, appearing worn out, humiliated, and desperate.
He required a powdered herbal remedy costing approximately NT$7,500 (about $230). With his gaze fixed on the floor, he murmured, “Doctor, I truly can’t afford this.”
My heart ached. He reminded me of my younger self (striving diligently, yet quietly battling through struggles).
So, I attempted to assist him. Or at least, I believed I was being of service.
I proposed that he could purchase a non-regulated, less expensive herbal powder for NT$3,000 elsewhere. Same concept, reduced price. A “thoughtful” recommendation.
He departed feeling relieved. I left feeling proud of my empathy. I shouldn’t have.
**The compassion that nearly caused harm**
Later on, I discovered more about the unregulated product I had recommended:
– Some batches exhibited microbial contamination.
– The concentration of active ingredients was erratic.
– Patients reported varying effects (and in rare instances, adverse effects).
My “kindness” had put him at risk. And if anything had transpired, both of us would have been unprotected (medically, ethically, and legally).
That night, I struggled to sleep. I replayed the interaction in my mind, grappling with a question I had shunned for years: “Is compassion truly compassion if it endangers the patient?”
**What I wish I had grasped earlier**
I entered the medical field believing that compassion was more important than rules. However, medicine taught me differently.
To my astonishment, boundaries (which I thought rendered a doctor “cold” or “inflexible”) were, in fact, a safeguard, a framework for safety and trust.
I once viewed diagnosis as merely a technical skill. Now I perceive it as a moral responsibility.
I previously thought flexibility equated to kindness. Now I realize that clarity equates to accountability.
I once assumed saying “yes” was a sign of caring. Now I recognize that sometimes: the most compassionate response a physician can offer is “No.”
**The deeper lesson behind an ancient saying**
In TCM, we refer to Da Yi Jing Cheng (“great physician, pure integrity”). For years, I regarded it as a poetic expression.
But I now interpret it differently:
– Integrity is not just a concept; it is a boundary.
– Compassion is not merely tenderness; it is discipline.
– Mastery is not only knowledge; it is restraint.
When compassion ventures into risky territory, it ceases to be compassion. When sincerity disregards safety, it turns into harm.
That young patient not only tested my judgment; he reshaped my understanding of what it means to truly care.
**What I will carry forward**
Whenever I encounter a tough decision now, I reflect on him. And I remind myself: A physician’s heart should radiate warmth. But a physician’s judgment must remain unwavering.
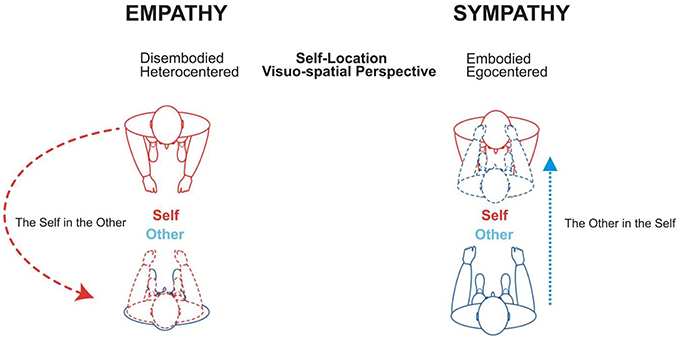
That equilibrium (between empathy and responsibility, between caring and safeguarding) constitutes the essence of medical practice.
Perhaps that is the lesson Da Yi Jing Cheng aimed to impart all along.
Gerald Kuo, a doctoral student in the Graduate Institute of Business Administration at Fu Jen Catholic University in Taiwan, focuses on health care management, long-term care systems, AI governance in clinical and social care environments, and elder care policy. He collaborates with the Home Health Care Charity Association and maintains a professional presence on Facebook, where he shares insights on research and community initiatives. Kuo assists in managing a day-care center for older adults, working closely with families, nurses, and community physicians. His research and practical endeavors aim to alleviate administrative burdens on clinicians, enhance continuity and quality of elder care, and establish sustainable service models through data, technology, and interdisciplinary collaboration. He has a particular interest in how emerging AI tools can assist aging clinical workforces, improve care delivery, and foster greater trust between health systems and the public.