Title: Adopting Innovation in Substance Use Disorder Treatment: The Potential of Contingency Management
As its term draws to a close, the Biden administration has implemented a significant policy adjustment aimed at enhancing outcomes for those facing substance use disorder (SUD). This initiative, praised by addiction professionals and healthcare practitioners, has raised the annual limit on Medicaid reimbursements for contingency management—an essential, evidence-backed behavioral strategy recognized for its demonstrable success.
This policy modification signifies an increasing awareness that creative, personalized treatment methods must supplant outdated, standardized approaches in addiction care. With more than 48 million Americans encountering SUD in the past year and relapse rates stubbornly high—ranging from 40% to 60%—the urgency for more effective, scalable strategies like contingency management is greater than ever.
Comprehending Contingency Management
Contingency management (CM) is grounded in behavioral psychology and is based on a straightforward yet compelling principle: rewarding individuals for positive actions to promote their recurrence. These incentives—often given as vouchers or digital micro-payments—are granted when patients achieve defined, attainable objectives, such as attending sessions, finishing therapy modules, or submitting drug-free urine samples.
This methodology is particularly effective for individuals with SUD because it engages the brain’s reward system. For those fighting addiction, immediate satisfaction from substance use frequently outweighs long-term advantages. Contingency management counters this tendency by providing immediate, positive reinforcement for healthy decisions.
The Research Supporting CM
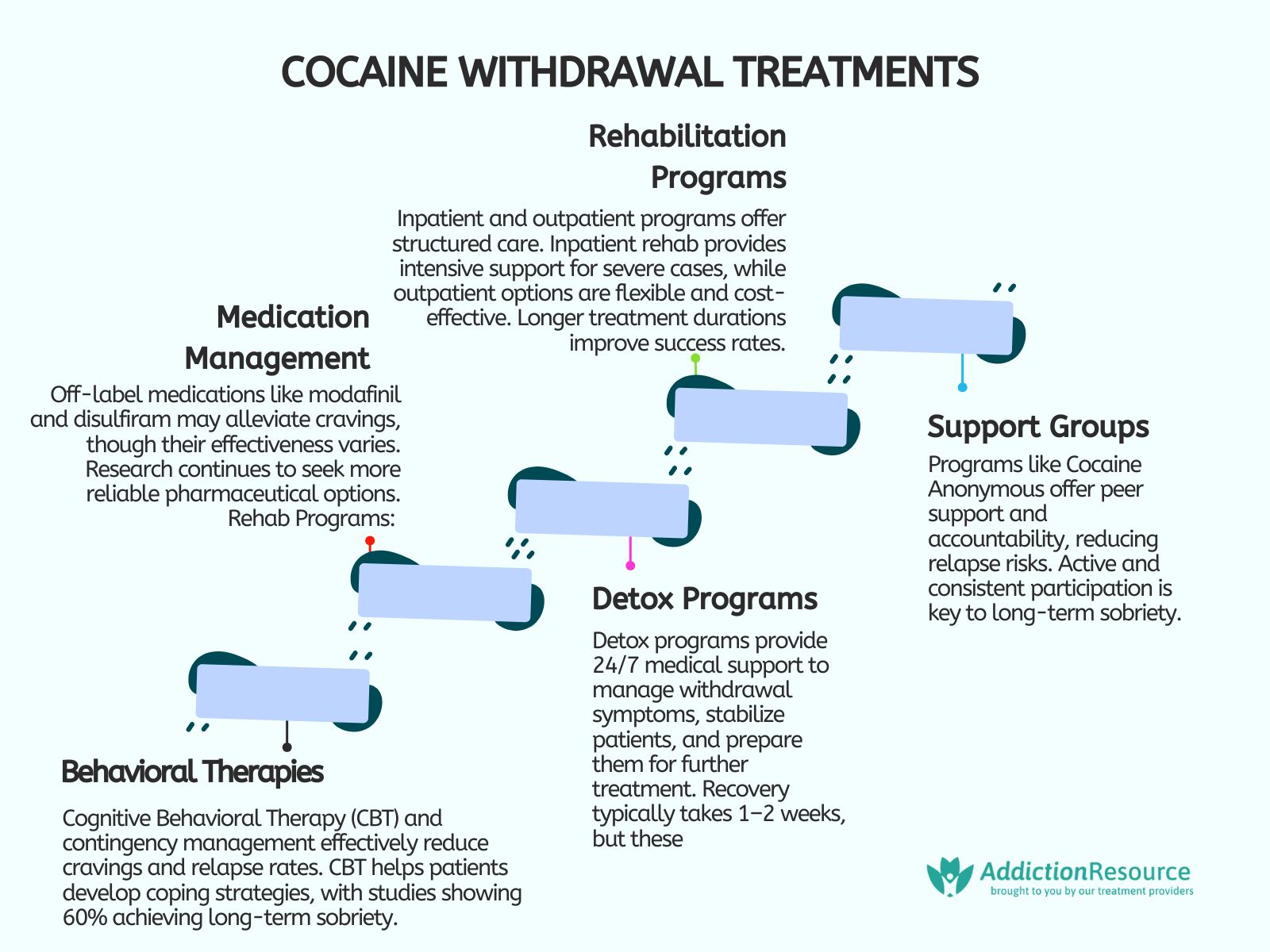
Numerous studies have confirmed the efficacy of contingency management in tackling stimulant use and various forms of addiction. Whether implemented in the context of cocaine, methamphetamine, or alcohol use disorders, CM consistently enhances retention in treatment and diminishes substance use.
Programs incorporating CM show not only increased participation but also improved outcomes overall. In instances like Jamie (name changed for confidentiality), who initially resisted therapy but became more committed after receiving small financial incentives, the advantages extend beyond mere compliance—they cultivate deeper therapeutic relationships, enhance self-esteem, and bolster long-term recovery.
Practically Implementing CM
The advancements in contemporary technology have rendered the implementation of contingency management more achievable and versatile than ever. Providers can collaborate with digital health platforms that automate reward systems, alleviating administrative burdens and effectively scaling care.
Applications like Noom, Holon Health, and other app-based platforms are already utilizing contingency management to enhance outcomes in mental health and addiction recovery. These applications streamline structured objectives, daily check-ins, and biometric data tracking to assist patients in maintaining their progress. For healthcare professionals, they deliver real-time insights into patient behaviors and engagement trends, enabling more tailored interventions.
Importantly, these systems are not limited to SUD treatment providers. Primary care physicians, mental health experts, and even criminal justice programs can engage with CM platforms to reinforce positive behaviors tied to health, abstinence, or adherence to court-mandated treatment plans.
A Contemporary Vision for SUD Treatment
Contingency management represents a more extensive transformation in how addiction care is approached. To address the complex and diverse needs of individuals with SUD, the field must adopt a future driven by technology, positive psychology, and precision medicine.
Artificial intelligence, for instance, can assist in crafting adaptive treatment strategies based on an individual’s history, conditions, and progress. AI-driven algorithms may ultimately forecast relapse risks and propose timely interventions, providing assistance before a crisis arises. Paired with wearable biosensors, these systems could reshape how we monitor and support recovery, heralding a new era of proactive, responsive care.
In conjunction with digital tools, the treatment landscape must progress to incorporate emerging pharmacological and holistic interventions. GLP-1 receptor agonists, once deployed for diabetes and obesity, are currently being examined for their potential to diminish cravings. Psychedelic-assisted therapies involving compounds such as ketamine, psilocybin, and MDMA are showing promise in rewiring the brain’s reward systems and addressing trauma—common underlying contributors to addiction.
Supporting therapies like transcranial magnetic stimulation (TMS), vagus nerve stimulation (VNS), and neurofeedback are also revealing early positive results. These neuromodulation techniques can alter brain activity and aid emotional regulation, stabilization of withdrawal, and cognitive restoration.
Furthermore, budding research into gut-brain axis interventions, peptides (e.g., BPC-157, NAD+), and adaptogenic substances suggests that a holistic recovery could be bolstered by targeting inflammation, stress response pathways, and cellular regeneration. Although still in the experimental phase, these methods signify progressive strategies that harmonize biology with behavioral health.
Transforming the Recovery Narrative
Historically, addiction treatment has centered on abstinence-focused programs, rigid frameworks, and stigmatizing terminology. Contingency management and other customized interventions challenge this model by providing hope and empowerment to individuals on their recovery journey.
The foundation for this new vision should be positive psychology—centered on strengths, advancement, and potential. When individuals feel encouraged, acknowledged, and celebrated for their accomplishments, no matter how minor, they are significantly more likely to remain engaged.