Title: The Painful Outcomes of Well-Meaning Actions: Reevaluating the CDC’s 2016 Opioid Recommendations
In response to a growing opioid crisis in the United States, the Centers for Disease Control and Prevention (CDC) released guidelines in 2016 designed to reduce prescription opioid consumption. The reasoning seemed straightforward: limit opioid prescriptions to prevent new addiction cases and ultimately decrease the number of overdose fatalities. However, as highlighted in Charles LeBaron’s book, Greed to Do Good: The Untold Story of CDC’s Disastrous War on Opioids, this well-intentioned initiative inadvertently caused significant harm to countless patients who genuinely needed relief, while failing to address the underlying causes of the opioid crisis.
A Guideline Founded on Insufficient Evidence
The 2016 CDC opioid prescribing guideline was based on a fragile scientific basis. While its main premises appeared logical—particularly the notion that prescribed opioids were a significant gateway to addiction—those involved in creating the guideline openly acknowledged the lack of solid evidence linking decreased prescribing with lower rates of addiction or overdose. Internally, the guideline’s foundational data was deemed “low” quality, indicating that the body of evidence presented considerable limitations and inconsistencies.
Nevertheless, the CDC moved forward with its recommendations with notable inflexibility. For acute pain, a mere three days of opioid therapy was recommended, extending to seven days only in exceptional cases. Chronic pain prescriptions were limited to 50 morphine milligram equivalents (MME) per day, with a theoretical maximum of 90 MME beyond which caution was mandated—but essentially discouraged. These limits were largely classified as “Category A,” applicable universally—ironically, the highest recommendation level was assigned based on the weakest evidence quality.
From Suggested Guideline to Nationwide Directive
Though the guideline was technically optional, its impact quickly proliferated throughout legal, regulatory, and healthcare systems at a rapid pace. By 2018, 33 states had implemented laws aligned with the 2016 guideline. Federal agencies followed suit; both the Department of Veterans Affairs and Department of Defense adopted comparable standards. Medicare adjusted its reimbursement policies to align with the guideline, and private insurers like Cigna and Blue Cross introduced even stricter regulations.
Pharmacies and pharmacy benefit managers joined the trend, with companies such as CVS and Walmart imposing strict limits on opioid distribution. By mid-2019, 70% of U.S. Medicaid programs had instituted dosage-based restrictions, often removing clinical judgment. Most controversial was Oregon’s Medicaid program, which proposed tapering all chronic pain patients to zero opioid consumption—regardless of their health status.
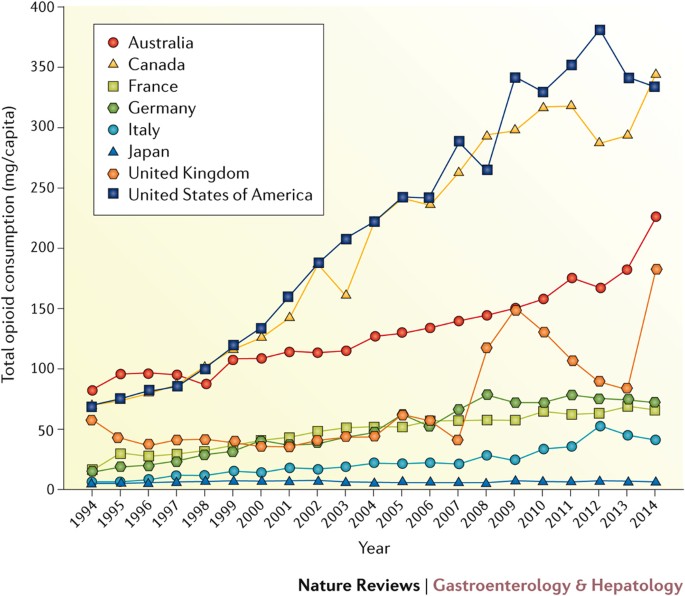
Severe Decline in Prescribing
Between 2016 and 2018, there was a significant drop in opioid prescriptions across various medical settings. Primary care providers reduced prescriptions by 40%, emergency departments by 71%, and even oncology specialists—who traditionally prescribed opioids for palliative care—reduced their prescribing by as much as 60%.
This steep decline might have been celebrated as a public health victory—had it not been for the subsequent surge in suffering.
Unintended Harm: Patients in Distress
Reports quickly emerged showing patients suffering from inadequate pain management, especially those with chronic health issues or terminal conditions. For veterans, the cessation of long-term opioid therapy was associated with increased rates of suicide and overdose deaths. One study indicated that abrupt dose reductions tripled the suicide risk in certain state Medicaid populations.
Cancer patients were also affected. A 2018 survey by the American Cancer Society indicated that nearly half of respondents faced obstacles in obtaining pain relief due to providers citing legal or insurance-related issues. Opioid prescriptions for cancer patients fell by 50% within just two years—a statistic alarming enough to imply systemic suppression of vital pain management.
Among the larger chronic pain population—comprising over 50 million Americans, with 17 million experiencing “high-impact” pain that disrupts daily activities—burden and despair escalated. A 2017 survey revealed that 95% of chronic pain patients felt the CDC guideline had negatively impacted them. A significant majority reported a decline in quality of life, increased pain intensity, and reduced daily functioning.
Physicians Restricted, Patients Neglected
Pain specialists and primary care physicians alike reported escalating pressures to comply. In a 2019 survey of pain doctors, 72% indicated they were compelled to reduce or deny opioid prescriptions to patients, even in medically necessary situations. Physicians expressed their frustration and anxiety. One anonymous doctor interviewed by Human Rights Watch described a climate of “absolute fear.” Consequences for non-compliance included professional repercussions or liability concerns, irrespective of individual patient circumstances.
The unintended results were neither abstract nor theoretical—they were tragic. Numerous anecdotal accounts and retrospective studies linked opioid tapering to suicides. In certain instances, patients faced three dire options: endure severe pain, resort to illegal street drugs, or take their own lives.
A Human Rights Emergency
In December 2018, the esteemed Human Rights Watch (HRW) provided a sobering analysis.