Title: Reevaluating Schizophrenia Therapy: The Rising Significance of Long-Acting Injectable Antipsychotics
In recent years, mental health treatment has been steadily shifting towards a more tailored and comprehensive method in managing schizophrenia and other enduring mental health disorders. Growing awareness of the diverse clinical manifestations, intricate psychosocial issues, and varied patient experiences has prompted a transition away from traditional treatment practices. A key advancement in this developing care framework is the increased acceptance and use of long-acting injectable (LAI) antipsychotics.
Previously viewed as a last resort, LAIs are now being incorporated earlier into treatment regimens—some specialists even advocate for their use after a first psychotic episode. This changing perspective reflects not just updated clinical guidelines and research findings but also a wider commitment to improving treatment results and aligning with patients’ needs and preferences.
Guidelines and Research Support Early Adoption of LAIs
Historically designated for patients with a track record of poor medication adherence or recurrent relapses, LAIs are now endorsed by prominent psychiatric organizations as a feasible initial treatment approach. In 2019, the American Psychiatric Association (APA) revised its guidelines to recommend LAIs as a primary treatment option for schizophrenia. These recommendations aim to decrease the mortality, morbidity, and debilitating outcomes often linked with the disorder.
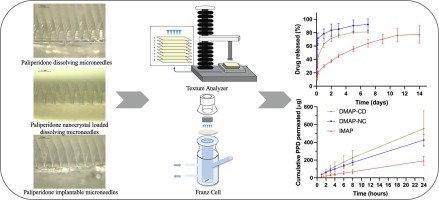
Numerous studies back this transition. LAIs have demonstrated enhancements in medication adherence, reductions in hospitalization rates, and improvements in overall functionality. Unlike oral antipsychotics, which necessitate daily ingestion, LAIs are administered by a healthcare professional at regular intervals ranging from two weeks to six months, depending on the specific medication. This not only ensures consistent therapeutic oversight but also addresses a persistent issue in psychiatry: accurately evaluating medication compliance.
The Advantages of LAIs in Schizophrenia Care
Managing schizophrenia extends beyond mere symptom control; it also encompasses reducing relapses, preserving cognitive health, fostering social inclusion, and aiding patients in sustaining their independence. LAIs present several therapeutic benefits that align with these objectives:
1. Enhanced Adherence: By decreasing the frequency of medication administration, LAIs eliminate a major obstacle to ongoing care. This is particularly advantageous for patients with limited insight or those facing challenges with executive functioning.
2. Fewer Relapses and Hospitalizations: Steady drug levels in the bloodstream help lessen the fluctuations often seen with missed doses of oral medications that can trigger relapses.
3. Improved Quality of Life: Medication-related decisions become less cumbersome, potentially fostering better adherence and allowing for mental energy to be directed towards recovery-oriented activities.
4. Alleviated Caregiver Stress: Caregivers are often crucial in ensuring treatment adherence. LAIs can help reduce the pressure of meticulously managing daily medication schedules, enhancing the caregiver relationship.
Barriers and Misunderstandings
Despite their therapeutic advantages, LAIs remain underutilized, mainly due to persistent stigma and misconceptions. Common misunderstandings include the belief that LAIs are uncomfortable, less effective compared to oral medications, or suitable only for patients with severe conditions. Furthermore, some professionals hesitate to suggest LAIs, fearing that patients might reject injectable therapies.
However, clinical experiences show that when LAIs are introduced in a supportive, informative, and patient-focused manner—particularly as an empowering alternative rather than a punitive step—many patients are willing to consider them.
Strategies for Moving to LAIs
Transitioning a patient from oral antipsychotics to an LAI requires collaboration, education, and thoughtful planning. Recommended practices include:
– Positive Framing: Present the injectable as a contemporary, low-maintenance treatment choice. Clinicians can phrase it as, “How do you feel about taking your medication just once every month or two, instead of every day?”
– Addressing Concerns: Patients should receive clear details about the injection process, duration of action, potential side effects, and insurance coverage.
– Collaborative Decision-Making: Involve patients and caregivers in a shared decision-making process, ensuring all perspectives are acknowledged and valued.
– Tailored Transition Plans: Not every patient may be ready for an immediate transition. Some might need to stabilize on oral medication first, while others could be prepared to begin an LAI during or after hospitalization.
The Future of LAIs in Mental Health Treatment
With advancements in formulation and accessibility, LAIs are gaining broader acceptance in psychiatric environments. Insurers are recognizing their role in reducing high-cost hospitalizations, and several states are simplifying the prior authorization process to enable easier prescribing.
As the mental health field continues to progress, LAIs are expected to take on a more significant role—not merely as a response to nonadherence but as an integral part of a proactive treatment philosophy focused on promoting long-term stability and wellness.
Conclusion
Schizophrenia is a complex, lifelong disorder that demands nuanced, multifaceted treatment. Long-acting injectable antipsychotics provide an appealing combination of clinical effectiveness, convenience, and patient empowerment. By normalizing discussions surrounding LAIs and more fully integrating them into care protocols, mental health professionals