Title: Functional Precision Oncology: The Personalization Revolution in Cancer Treatment
Within the transforming realm of cancer therapy, functional precision oncology (FPO) is reshaping our strategy toward one of contemporary medicine’s most daunting obstacles. While conventional precision medicine focuses on genetic alterations and genomic analysis, FPO elevates the idea of personalization to a more actionable, pragmatic level—by actively assessing how a patient’s tumor reacts to medications in vitro. This groundbreaking method promises to enhance treatment response rates, increase survival, lessen unnecessary side effects, and greatly cut healthcare expenses. However, it’s surprising that FPO is notably missing from most cancer treatment guidelines.
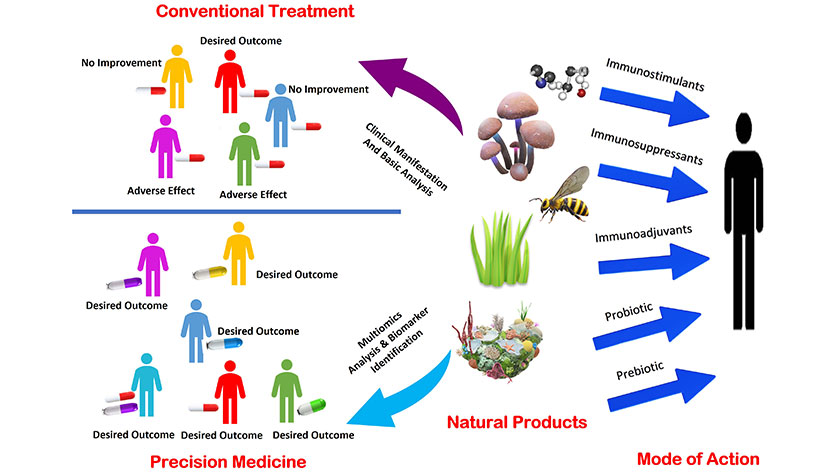
Recognizing the Shortcomings of Traditional Cancer Treatment
Conventional cancer treatment begins with pathology—the microscopic examination of a biopsy utilizing stains such as H&E to identify the cancer type. Although this critical step discerns the characteristics of the malignancy, it offers little insight into how the tumor will react to particular therapies. Most existing protocols depend on collective data: studies showing how a cohort of patients with similar cancers responds, on average, to a given treatment. Nevertheless, cancer is highly individualized, with each patient’s tumor displaying its distinct biological makeup.
Consider pancreatic cancer. If your health permits, you may be prescribed a chemotherapy regimen like FOLFIRINOX, which boasts a response rate of 32%. For patients in poorer health, gemcitabine combined with Nab-paclitaxel is the typical substitute—effective in about 24% of instances. This indicates that most patients face disease progression, enduring taxing side effects without any guarantee of benefit from the selected option.
Drawbacks of Genomics-Only Precision Medicine
The genomic revolution has profoundly influenced precision oncology by targeting “actionable mutations” that align with specific drugs. However, this strategy is limited by biological complexities. Dr. Keith Flaherty, professor of oncology at Harvard and chief investigator of the National Cancer Institute’s MATCH trial, notes that only approximately 25% of cancer patients possess mutations that link directly to FDA-approved drugs. Even in well-studied malignancies like HER2-positive breast cancer, introducing Herceptin raises response rates from 29% to 45%—a notable improvement, yet still not universally effective.
Genomic data offer vital insights, but a singular mutation fails to capture the diverse interactions taking place within a living tumor. Factors like drug metabolism, tumor microenvironment, protein expression, and unidentified mutations all contribute, thus reducing the predictive capability of a solely genomic approach.
Functional Precision Oncology: From Lab to Lifesaving Care
Functional precision oncology fills this void by directly evaluating how a living tumor sample reacts to a variety of treatments in a laboratory environment. This process is similar to antibiotic sensitivity testing used for infectious disease management—it’s evidence-based and tailored to the individual.
Pioneers like Sidney Salmon and Anne Hamburger in the late 1970s established this concept by culturing tumor cells and analyzing drug sensitivity. Subsequent advancements by Dr. Daniel von Hoff and Dr. Larry Weisenthal led to the creation of improved methods, such as differential staining cytotoxicity (DiSC) assays, to more accurately and efficiently discern effective therapies. These foundational approaches yielded promising results, often predicting clinical outcomes with over 80% accuracy. Nevertheless, challenges such as delayed turnaround times, labor-intensive procedures, and the complexities in culturing some tumors initially hindered broad acceptance.
The Rise, Fall, and Return of Functional Profiling
With the emergence of next-generation sequencing (NGS) in the early 2000s, functional profiling became less prominent. NGS provided convenience: it could be conducted on preserved specimens, was simpler to incorporate into pathology workflows, and closely aligned with pharmaceutical approval protocols. It rapidly gained recognition and was integrated into guidelines from bodies like the National Comprehensive Cancer Network (NCCN). Yet, numerous oncologists have expressed difficulty in deciphering these genomic reports, finding them clinically irrelevant without clear, actionable targets.
Currently, FPO is witnessing a revival. Advances in technology—especially in 3D microtumor modeling (organoids) and AI enhancements—have allowed ex vivo drug testing platforms to yield dependable results within 7 to 10 days. These predictions have shown strong correlations with actual outcomes in clinical trials, including notable survival improvements among glioblastoma patients influenced by functional testing outcomes. These instruments do not replace genomics—they serve to augment them.
Obstacles to Implementation
Despite its potential, functional precision oncology largely remains excluded from standard care protocols and significant guidelines such as those from the NCCN. Hospitals frequently limit external tissue testing, and financial and institutional frameworks within healthcare systems favor standardized methods over personalized ones. Physicians, particularly those at leading academic institutions, might be reluctant to embrace techniques that lack formal endorsement, regardless of supporting evidence for their efficacy.
This stagnation leaves many patients uninformed about FPO as an available alternative. In a time when personalization is transforming all facets of technology and lifestyle, it is remarkable that cancer care has yet to fully embrace this paradigm shift.