Title: The Rural Health Care Crisis Is More Than a Matter of Policy—It’s an Ethical Dilemma
By Dr. Pamela Buchanan
I am a physician trained in family medicine operating within a rural emergency department. Every shift begins with a 90-minute commute—not for the love of vistas or solitude, but because if I don’t show up, there may be no one available to care for the patients who come through the doors. The county I work in has already seen the closure of its main hospital. The obstetrics unit? Disappeared. Specialist assistance? Infrequent at best. And the patients? They are more unwell than they ought to be—a dire outcome of delayed diagnoses, insufficient management of chronic ailments, and systemic disregard.
What we are confronting is not an unanticipated emergency—it is a foreseen breakdown.
Since 2010, over 140 rural hospitals in the United States have closed their doors. Up to 600 more are presently in jeopardy. These shutdowns disproportionately harm our most at-risk populations—individuals who tend to be older, sicker, lower-income, and less insured compared to those living in urban settings. Enhancing the crisis, nearly 80% of rural counties are classified as Health Professional Shortage Areas. Yet, merely 4% of medical school graduates intend to serve in rural locations.
Why? Because rural medicine has become a test of endurance. It is underfunded, overtaxed, and politically undervalued. It can often be perilous. Nevertheless, despite all the hurdles, doctors, nurses, and technicians continue to arrive for duty.
Currently, academic-policy discussions and political influencers are exploring proposals that could shape the future, like Project 2025, which recommends substituting trained health care professionals with “volunteers” in rural regions. As if mere good intentions can accomplish tasks such as delivering babies, resuscitating trauma patients, or managing mental health crises in communities already on the brink.
This strategy isn’t merely naive—it’s hazardous. And lethal.
The stark realities I encounter daily reveal truths that policy papers often gloss over. Women hemorrhaging postpartum after delivering without prenatal care. Infants born in vehicles because the nearest labor and delivery facility is 100 miles away. Elderly individuals going months without medical consultations due to transportation barriers. These aren’t tales from a distant underdeveloped nation—they are occurring in contemporary America.
Maternal health services have been particularly ravaged. Between 2011 and 2021, over 200 rural hospitals eliminated their OB units. It’s not a coincidence that more than half of all U.S. counties currently lack a single OB/GYN. In the wealthiest nation in the world—one with the highest maternal mortality rate among developed countries—this is an abomination. For Black women, like myself, the risk is three times more severe.
I have lived through this nightmare from both the provider and patient perspectives. During my first pregnancy, I suffered from pre-eclampsia. Even as a medical student, I had to diagnose myself and insist on intervention. My education saved my life. Others are not as fortunate.
As a physician, a mother, and a Black woman, I cannot remain silent while our health care system systematically overlooks those who are in the greatest need. What we are witnessing is not only unsustainable—it is unethical.
We cannot continue to assume that this issue will improve with volunteer band-aids. Emergency departments do not operate on goodwill. Labor and delivery cannot function on mere optimism. The structural collapse of health care cannot be mended with catchy phrases.
We need substantial investments, such as:
– Increased loan forgiveness and scholarship programs that reward service in rural and underserved communities.
– Boosted funding for graduate medical education (GME) in rural residency programs, ensuring trainees are exposed to rural care and encouraged to remain.
– Sustainable reimbursement models that cater to community demands, not urban-centric algorithms.
– Fair pay to attract and retain nurses, medical assistants, social workers, and technicians where they are critically needed.
– Significant investment in broadband and telemedicine for regions where traveling hours for a check-up isn’t practical.
Moreover, we must protect and expand valuable initiatives like the Teaching Health Center GME, which face threats of funding cuts despite their proven effectiveness at placing doctors in urgently needed communities.
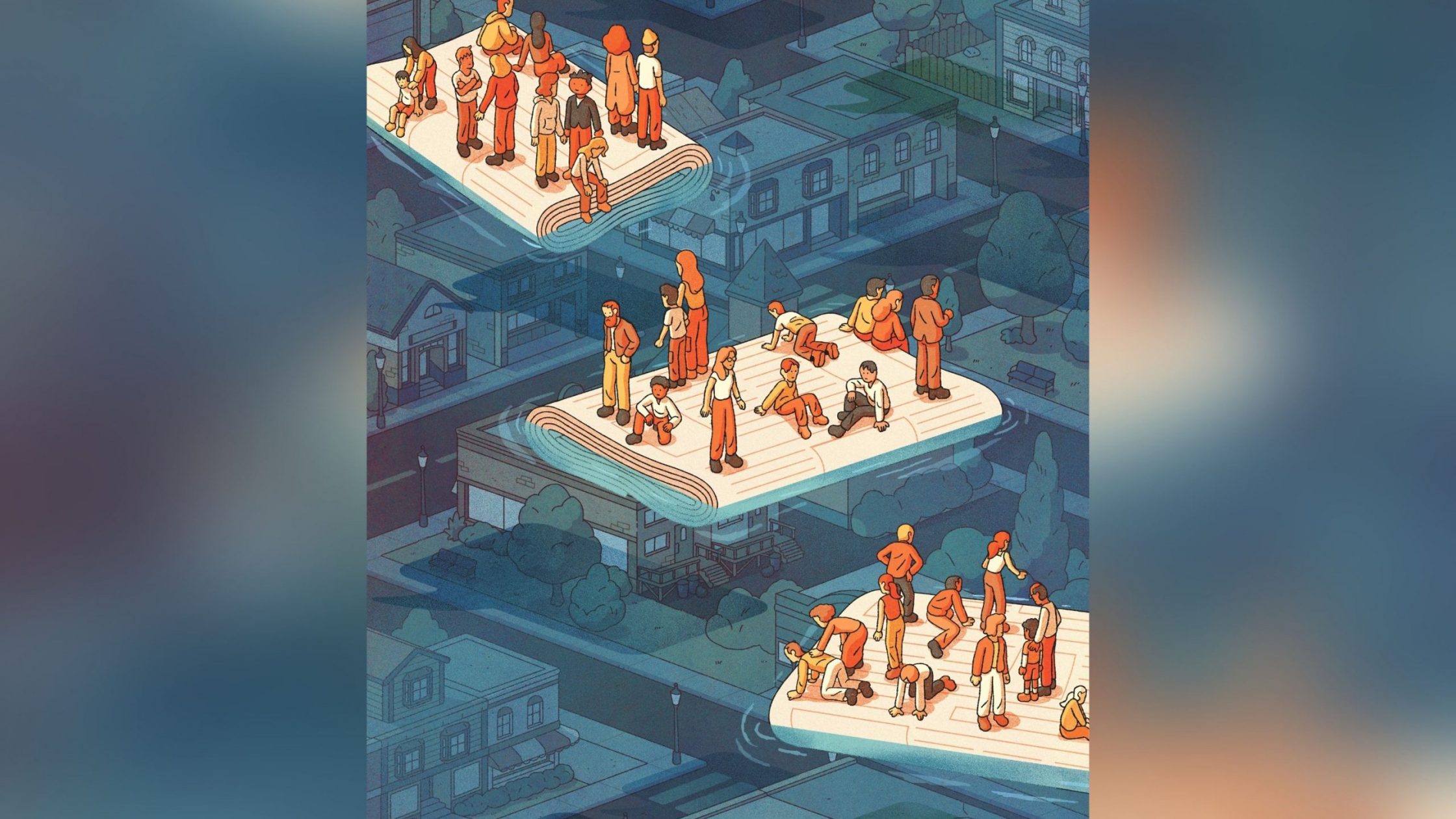
Rural care is not charity. It isn’t a privilege for the wealthy or a political issue—it is a fundamental, life-sustaining necessity. When we dismantle rural health care, we don’t merely lose service lines or personnel—we lose lives. Mothers, fathers, grandparents, children.
I didn’t become a physician to navigate political corridors, but the current moment calls for more than clinical expertise. It requires advocacy. Urgency. Accountability.
Because when the ultimate narrative is crafted, we will recognize that this was not an unfortunate coincidence or an inevitable result of geography. It was a decision—to allow entire communities to fall through the cracks while those in charge debated whether volunteers could fill the void left by a shrinking, fatigued workforce.
We can.