My name is Ava Kaufman, and my physicians did not believe I would be here today. I beat the odds after being placed on the list for – and undergoing – an experimental heart transplant.
Prior to my transplant, I was a healthy mother and entrepreneur with a passion for dance. I unexpectedly noticed a rash developing on my hands and shins, prompting a visit to the dermatologist. They diagnosed me with psoriasis, which progressively worsened and resulted in highly elevated muscle enzymes. I was referred to a rheumatologist for a muscle biopsy, during which I lost consciousness.
I was swiftly taken to Cedars Sinai, where I was immediately placed on life support. Fortunately, I lived only five minutes from the hospital. Had I been further away, I might not have received the critical treatment I required. The doctors identified that I had a rare autoimmune disorder known as dermatomyositis.
This illness severely compromised my heart – a situation the doctors had never encountered before. My only chance of survival, which they considered minimal, was to undergo a heart transplant. While facing death, I made a pact with God that if I survived – if I could have more time on Earth with my daughter, Jade – I would dedicate myself to giving back to my community for the remainder of my life. I was fortunate enough to receive a heart transplant in time to preserve my life. Interestingly, the surgery occurred on my birthday.
To fulfill the promise I made with God, I established [Ava’s Heart](https://avasheart.org/), a nonprofit organization that provides essential support to organ transplant recipients lacking access to necessary resources. The transplant journey does not conclude once a patient is matched with an organ. Recipients face rising expenses, seemingly endless tests, and logistical challenges before, during, and after the transplantation process.
**Beyond the match: Transplant housing posing a barrier**
To even qualify for a transplant, patients must either reside close to or be capable of traveling to a major hospital or transplant center where the operation will take place. If they cannot secure arrangements within a 30-minute radius, for instance, they will be unable to undergo the transplant they urgently require. Through my own experiences, I learned that if a patient is unable to afford housing near their transplant center for at least three months post-transplant, they cannot proceed with the surgery.
Post-transplant housing is not typically covered by insurance, and very few hospitals offer it. During my recovery, I met families sleeping in their cars in the parking garages of transplant centers for months due to the high cost of local housing, as well as those who, unfortunately, returned home without their transplant.
I made it my mission to find housing solutions in Los Angeles to help alleviate the burden on transplant recipients, from funding hotel stays to leasing houses for them during their post-transplant recovery. It is necessary to address inequities within the transplant community and make transplantation more accessible and practical so that patients can obtain the vital care they need.
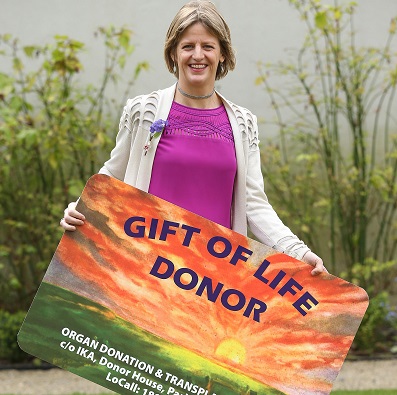
**Organ donation saves lives.**
As additional patients are added to the transplant list each year, the demand for organs is exceeding the current supply. A fundamental step in closing the supply and demand gap is to promote organ donation; it is one of the most heartfelt ways to give back. By donating an organ, you grant someone, like me, a second chance at life.
At 75 years old, I often reflect on the nearly 16 years since my procedure, and I am truly thankful that my transplanted heart is thriving, and that I am fortunate to share my story today. With increased organ donation, we can improve the prospects of providing patients with hope. As I remind others, souls ascend to heaven, but organs remain here.
*Ava Kaufman is a patient advocate.*