Exploring the Dynamics of Trust in the Physician-Patient Relationship
The relationship between a physician and a patient is fundamental to effective healthcare. Historically, patients have frequently placed considerable trust in their doctors, demonstrated by remarks like “Whatever you say doc, I know you will do right by me.” Such statements reflect the trust and confidence that patients have conventionally granted to their healthcare providers. Nevertheless, the nuances of this trust are changing due to various societal and systemic transformations.
The decline of trust in the medical field can be linked to a transition from paternalistic care models to more collaborative frameworks. While this change encourages patient participation in health decisions, it also aligns with an increase in skepticism and challenges to medical authority. Patients are more frequently turning to online resources like Google, occasionally utilizing this knowledge to question or dispute their physician’s recommendations. This pattern underscores a growing necessity for physicians to navigate the intricacies of maintaining trust while interacting with informed and at times cynical patients.
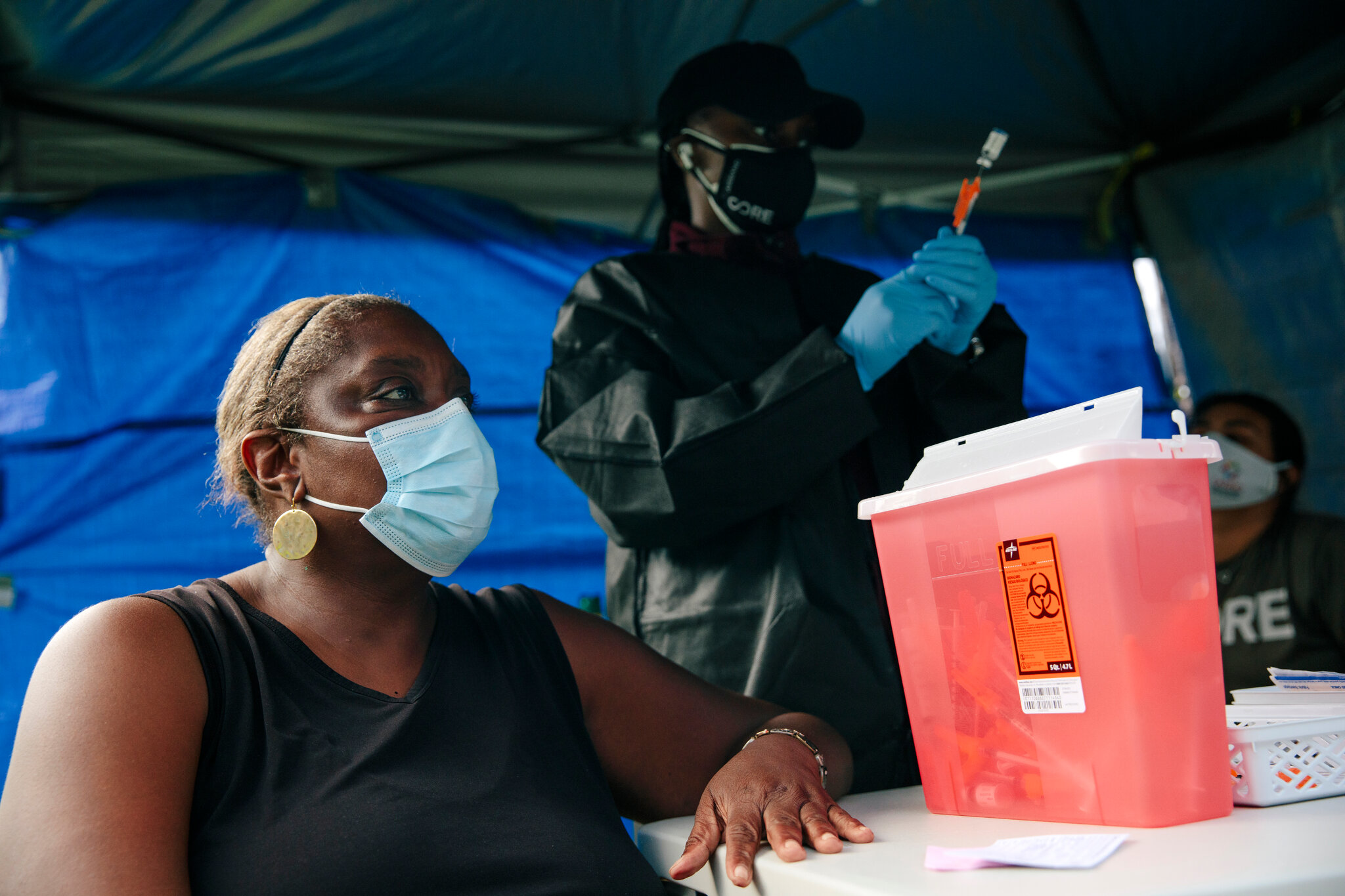
Factors contributing to this shift include a wider societal skepticism towards expertise, intensified by the COVID-19 pandemic. The pandemic has brought attention to disparities and inconsistencies in healthcare information, leading to a mistrust of medical guidance. Furthermore, physician conduct on social media has at times fueled this skepticism. Additionally, systemic issues within healthcare, such as the devaluation of primary care roles and shortened appointment times, have restricted opportunities for meaningful exchanges between doctors and patients. Such limitations can obstruct patients’ ability to voice their concerns and hinder physicians’ capacity to deliver attentive care.
In spite of these obstacles, surveys reveal that individual patient trust in their physicians remains fairly strong. This persistent trust is crucial, especially in light of recent events like the surprising termination of members of the Advisory Committee on Immunization Practices (ACIP). The replacement of these experts with less qualified individuals who hold controversial views has heightened worries regarding the erosion of trust in institutional expertise. Physician associations have reacted promptly, advocating for the reinstatement of ACIP members and contesting decisions they view as detrimental to public health.
Given these circumstances, sustaining trust necessitates continuous engagement with professional organizations like the American College of Physicians, which follow strict, evidence-based guidelines. Initiatives such as the Vaccine Integrity Project aim to reinforce confidence in vaccine information and act as a reliable source for the public. Moreover, a transformation in communication approaches is essential, moving away from conventional top-down models towards more direct and impactful methods of public interaction.
Safeguarding the vital trust between patients and physicians requires efforts to support policies that promote transparent and empathetic healthcare practices. It also means upholding ethical standards demonstrated by individuals like Paul Farmer, whose work focused on building trust “one patient at a time.” As the largest medical specialty organization in the United States, the American College of Physicians champions this cause, striving to deliver compassionate, informed care to nurture lasting trust in medical professionals.