It is occurring more frequently than many realize. The same doctors who appear unwavering in the operating room or clinic, those who navigate chaos without flinching, are discreetly arranging therapy sessions. Not because they have “hit rock bottom” or can no longer perform their duties, but because they are understanding they do not have to bear it all alone. Nor can they endure this degree of burnout any longer.
As a psychologist who works with physicians, I witness this transition firsthand in my therapy practice. In recent years, an increasing number of doctors are reaching out. And not solely because they are in full-blown crisis, but because they are recognizing the need for something deeper; a space to navigate and reflect on the human aspects of their experiences as a physician and their existential purpose in life beyond medicine. This isn’t about weakness. Quite the opposite. Instead, it is about finally allowing themselves the opportunity to seek help.
Why now?
I observe several converging trends:
1. Burnout is no longer a taboo phrase. Not long ago, acknowledging burnout could feel like a career-ending admission. Now, however, more physicians are candidly discussing burnout with their colleagues, whether at happy hour post-call, at conferences, with friends and family, or in articles like this one. They are no longer willing to silently endure the symptoms of burnout. This openness and vulnerability thankfully facilitate the subsequent step: pursuing therapy before burnout spirals out of control.
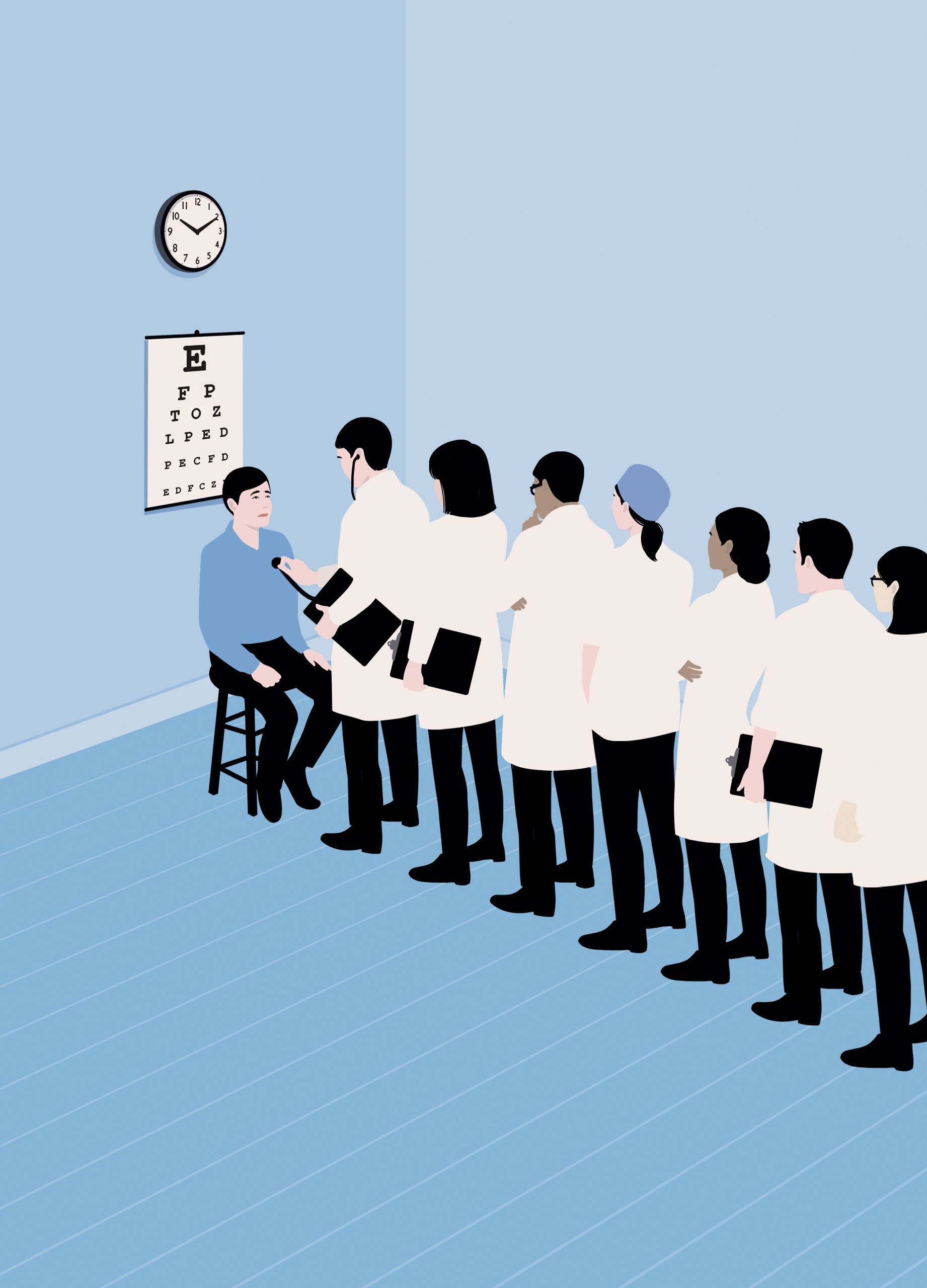
2. The “invincible doctor” myth is fracturing. Medical culture has traditionally valued stoicism, the capacity to work through exhaustion, grief, personal issues, and internal conflict without revealing any signs. Yet more doctors are beginning to question whether this is feasible, or even beneficial. Thank goodness for that.
3. Shifts in generational mindset. Younger physicians have grown up with a culture of greater openness, honesty, and straightforwardness regarding the significance of recognizing and caring for one’s mental health. They are less inclined to view therapy as a last resort and more apt to consider it a regular form of self-care, akin to going to the gym or the necessity of annual check-ups.
4. The pandemic shattered the silence. COVID-19 served as a pivotal moment for conversations around mental health in general, particularly for physicians. It dismantled the illusion that doctors can remain unaffected by constant exposure to suffering, moral dilemmas, systemic issues, chronic overwork, uncertainty, trauma, and more. For many, it marked the first time they acknowledged: “I can’t keep doing this without assistance.” and “I deserve better; I don’t have to continue living like this.” They are prepared to genuinely address their burnout, instead of suffering in silence.
What physicians seek in therapy
Physicians seldom arrive at therapy asking for generalized “stress management techniques.” In fact, they usually already possess that knowledge—they spend all day advising their patients on the same strategies, after all. Instead, they are in search of:
A safe environment to speak candidly. There is often an expectation to remain composed and collected that doctors experience when interacting with patients, trainees, and even family. In therapy, doctors can shed the façade and start connecting with their authentic selves.
A therapist who comprehends their reality. Doctors prefer a therapist who grasps the unique challenges of medicine without requiring a lengthy preamble about why a negative outcome still troubles them. Many of the physicians I encounter express relief at finding a therapist who doesn’t necessitate spending more time elucidating the realities of medicine instead of actually discussing and delving into the difficulties they are there to address.
Depth rather than quick solutions. The physicians I work with often desire to investigate the deeper reasons for their feelings of discontent or disconnection, even (and often especially) when their careers appear impactful on paper.
Why “quietly” matters
For better or worse, many physicians who begin therapy do not advertise it. They may inform a close friend or partner, but they are not proclaiming it in the staff lounge. The subtlety may occasionally stem from shame or stigma surrounding mental health care, yes. But it can also be grounded in the same instinct that prevents a doctor from sharing intimate personal details with colleagues; managing TMI. Nonetheless, even discreet participation can create ripple effects. I’ve had clients reveal that, months later, a colleague confided they were in therapy too, and suddenly, there was a sense of shared permission to be more human at work.
Therapy as a professional investment
Some physicians commence therapy because they are teetering on the edge of leaving medicine. Others seek therapy because they wish to remain in their careers, but no longer at the cost of their mental health, relationships, or sense of self. Still others pursue therapy because they are finally ready to acknowledge that persistent feeling within that something isn’t right and that it’s time to seek support to explore what that entails.