Memory impairment is a widespread and frequently troubling issue in the medical field. Recent innovations over the last five years have greatly enhanced the assessment of cognitive decline. Healthcare providers are no longer restricted to simply excluding dementia; they now have advanced tools to identify early signs of Alzheimer’s disease and other neurodegenerative disorders before significant symptoms emerge, empowering patients to make educated choices regarding their futures.
The initial phase in assessing memory impairment involves a thorough history-taking, which includes conversations with both the patient and a close companion, usually a spouse. This conversation aids in revealing subtle shifts in cognition or daily activities that may not be noticeable to the patient. Subsequently, a targeted neurological evaluation, which includes cognitive assessment using instruments like the Mini-Mental State Exam (MMSE), is performed to distinguish Alzheimer’s disease from other comparable disorders such as Lewy body dementia or dementia associated with Parkinson’s disease. It is noteworthy that as many as 40 percent of patients with Alzheimer’s may develop parkinsonism, which can influence diagnosis and treatment.
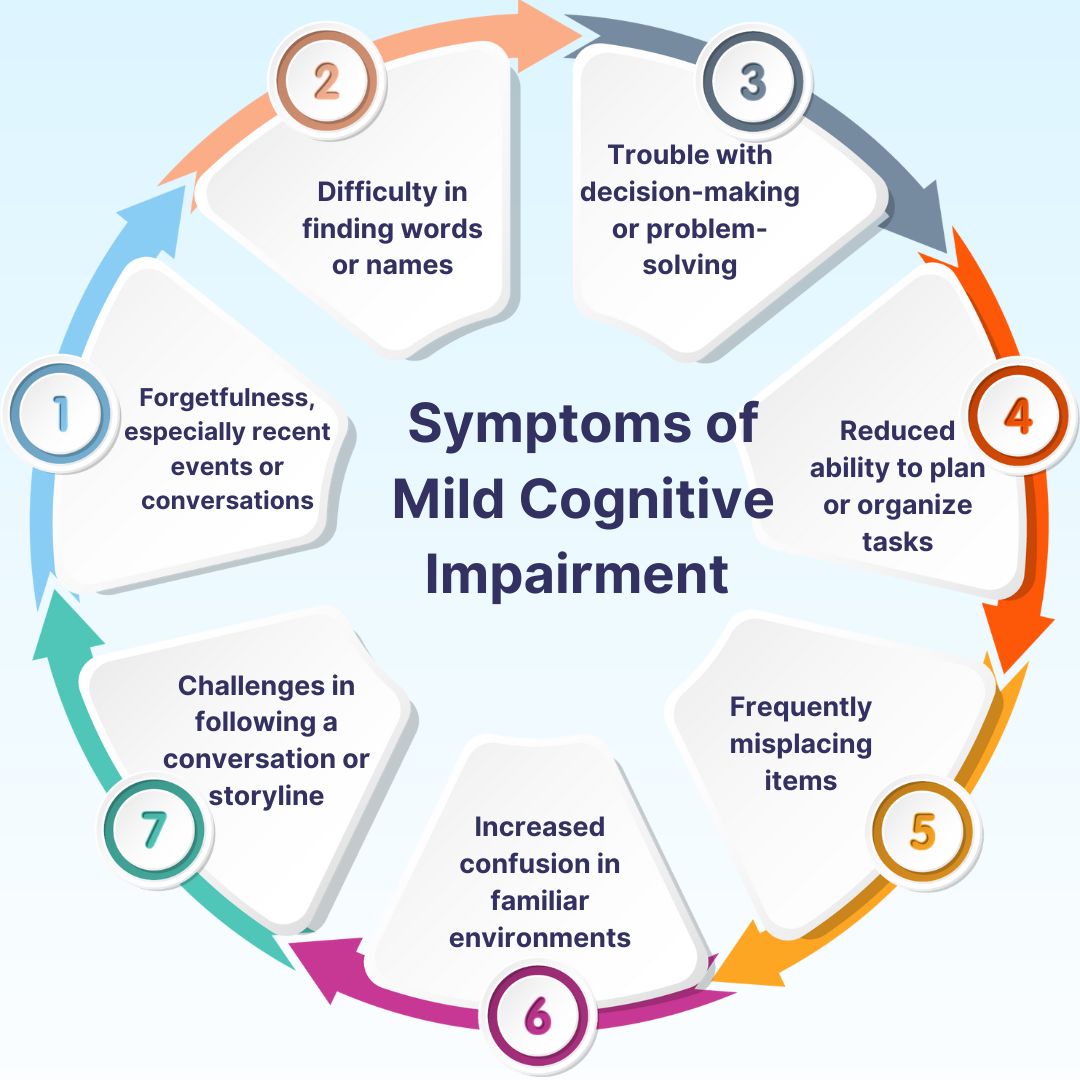
Mild cognitive impairment (MCI) is acknowledged as a separate diagnosis, situated between typical aging and dementia. Individuals with MCI exhibit measurable cognitive alterations; however, these changes do not drastically affect daily living initially. The prognosis differs: approximately half of the patients maintain stability, while others may progress to dementia, requiring continuous monitoring and follow-up.
Objective assessments facilitate diagnosis, with high-resolution MRI identifying structural alterations in the brain and EEG used to exclude seizures. Amyloid PET imaging reveals amyloid accumulations, a significant pathology of Alzheimer’s, although it is not definitive on its own. Laboratory evaluations are crucial to eliminate reversible causes, incorporating tests for thyroid function, vitamin B12 levels, and inflammatory markers. New blood biomarkers are now available, providing high accuracy in recognizing early Alzheimer’s pathology.
Tailored treatment follows the clarification of the diagnosis. Oral medications like donepezil or memantine are commonly prescribed for cognitive enhancement. Intravenous anti-amyloid treatments may be utilized to slow disease progression, with patients frequently directed to specialized facilities for such therapies. Additional medications for mood or anxiety disorders, along with lifestyle interventions like physical activity and social interaction, are vital for sustaining function.
The early identification of Alzheimer’s disease affects more than just pharmacological treatment; it enables proactive life planning. Patients have the chance to make choices about work, driving, finances, and estates while they are still capable. As a neurologist, leading patients through this journey is immensely rewarding, as it grants them clarity and control over their future during what may be an uncertain period.
Evaluating memory impairment today encompasses a comprehensive, individualized method that integrates history, examination, imaging, EEG, lab tests, biomarkers, and therapies customized to the patient’s biological and life situation. These contemporary diagnostic tools facilitate early disease identification, proactive interventions, and enhanced quality of life, merging scientific accuracy with compassionate patient care.