### The Initial Loss: Contemplations on a Young Patient, Medical Progress, and the Legacy of Research
The deep emotional and ethical impact of losing a patient is an experience that lingers with doctors throughout their professional journeys. For Dr. Richard D. Sontheimer, this unforgettable moment occurred in the 1970s during his advanced medical training at an academic hospital in the western United States. Even after nearly fifty years, Sontheimer vividly recalls the young mother of three who tragically succumbed to metastatic malignant melanoma while under his care—a somber reminder of both the fragility of human existence and the progress that medicine has achieved since that time.
This scenario represents not only a personal reminiscence but also an exploration of the incredible advancements in cancer therapy over the last fifty years. It emphasizes how breakthroughs like immune checkpoint inhibitors have redefined survival possibilities, highlighting the vital role of ongoing biomedical research.
—
### The Patient: Battling Against the Odds
Dr. Sontheimer’s patient was an energetic young woman, married and the mother of three small children. She was brought to the hospital after suffering from frequent seizures. Further investigation revealed a history of malignant melanoma, raising concerns about whether the seizures were symptomatic of a potentially treatable neurological issue or brain metastases resulting from melanoma. Regrettably, diagnostic technologies like CT scans were not commonly accessible at that time, which hindered timely and conclusive assessment.
Standard X-rays ultimately verified the existence of a significant metastatic tumor in her brain. In the 1970s, metastatic malignant melanoma had a dismal prognosis, with five-year survival rates falling below five percent. Lacking effective chemotherapy alternatives, surgery was considered her most viable option for extending her life. The surgical removal of the tumor provided her with an additional six months before the complications of her illness took her life.
Though the result was heart-wrenching, her situation powerfully illustrates the extraordinary strength and determination of patients grappling with overwhelming challenges—and how restricted medical interventions were just a few decades ago.
—
### Medical Progress: A New Chapter in Treating Metastatic Melanoma
If that courageous young mother had received care today, her survival chances would have improved significantly due to the introduction of immune checkpoint inhibitor therapy. These innovative drugs represent one of the most significant breakthroughs in contemporary oncology.
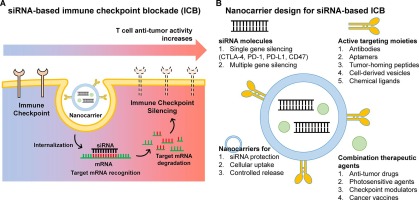
The human immune system is designed with “stop and go” mechanisms, which help it to recognize and eliminate threats like cancer cells without becoming overactive and harming healthy tissues, a condition that could lead to autoimmune diseases. Immune checkpoint inhibitors function by disabling the “stop” signals, thereby enabling the immune system to proactively seek out and eradicate cancer cells.
Medications like nivolumab and ipilimumab, both immune checkpoint inhibitors, have revolutionized the treatment paradigm for patients with advanced melanoma. These treatments have produced results that were once beyond imagination in advanced cancer cases.
A notable landmark study titled *”Final, 10-year outcomes with nivolumab plus ipilimumab in advanced melanoma,”* published in the *New England Journal of Medicine*, highlights the impressive benefits of this strategy. The research tracked 945 international patients over ten years, revealing that those who received both medications had a median survival of 71.9 months (almost six years), with median melanoma-specific survival surpassing an incredible 10 years. These figures represent nothing short of a groundbreaking enhancement when compared to survival outcomes from the 1970s.
Immune checkpoint inhibitor therapy has provided patients with the opportunity to live beyond the bleak outlooks they would have encountered in earlier times—time to connect with loved ones, witness important life events, and craft their own stories, instead of having their narratives prematurely cut short by illness.
—
### The Cost of Advancement: Navigating the Challenges of Contemporary Healthcare
As remarkable as immune checkpoint inhibitor therapy is, it symbolizes an unsustainable financial trajectory in modern American medical care. Presently, the annual expenditure for this therapy ranges from $100,000 to $300,000 per patient in the United States—a statistic that underscores the conflict between medical breakthroughs and economic realities.
Dr. Sontheimer aptly refers to this dilemma as a “many-headed monster” of rising healthcare expenses. Any movement toward reforming the system necessitates collaboration and negotiation among all involved parties. Nonetheless, one crucial element should not be compromised: the relatively modest cost of supporting fundamental and clinical biomedical research within academic and scientific institutions. Research efforts serve as the delicate foundation from which transformative treatments like immune checkpoint inhibitors are developed.
Without a sustained commitment to investing in forefront scientific inquiry, advancements like these—ones that transform survival expectations and provide hope to the most desperate patients—would be unattainable. Any reform initiatives must balance the necessity of cost management with the critical need to safeguard the innovations that have fundamentally altered the landscape of modern medicine.
—
### Connecting the Past and the Present: The Human Spirit and Medical Science
Dr. Sontheimer’s recollections of his formative years in medicine highlight the convergence of technology