# The Future of Psychiatry: Innovations and Challenges in the 21st Century
In the 21st century, psychiatry is more important than ever. As our ways of living change and the global economy shifts to a knowledge-centric model, ensuring mental well-being has become pivotal for attaining personal and professional achievements. Psychiatry is essential in enhancing cognitive and emotional well-being, allowing individuals to enjoy healthier, more fruitful lives.
Dr. Benjamin Rush, regarded as the father of American psychiatry and a signer of the Declaration of Independence, famously remarked, *“Temperate, sincere, and intelligent inquiry and discussion are only to be dreaded by the advocates of error. The truth need not fear them.”* This perspective continues to hold significance as psychiatry adapts alongside scientific progress, integrating new methods and techniques to bolster diagnostic precision and treatment effectiveness.
## The Distinctive Diagnosis Challenges in Psychiatry
Despite notable progress in medical science, psychiatry still heavily depends on subjective accounts from patients, clinical observations by physicians, and pattern recognition for diagnosing and treating disorders. Unlike other medical fields, psychiatry does not utilize standardized diagnostic methods such as blood tests, physiological evaluations, or imaging modalities typically found in cardiology, endocrinology, and neurology.
Consider the scenario where cardiologists depended entirely on self-reported indications without utilizing electrocardiograms (EKGs), echocardiograms, or blood analyses. Such a methodology would appear antiquated and inadequate. Given the intricate nature of the human brain, psychiatry continues to encounter significant obstacles in creating objective diagnostic instruments. Nevertheless, encouraging strides in genetics, biomarkers, neuroimaging, electrophysiology, and artificial intelligence (AI) are clearing the path for a more accurate and scientifically grounded mental health care system.
## Genetics’ Contribution to Psychiatry
One of the most thrilling developments in psychiatry is the incorporation of genetic research into clinical settings. Psychiatric genomics has permitted the identification of genetic indicators associated with mental health disorders like depression, bipolar disorder, schizophrenia, autism spectrum disorder, and attention deficit hyperactivity disorder (ADHD). Though the field remains nascent, insights from genetics are allowing researchers to grasp individual vulnerabilities to these illnesses.
Pharmacogenomics, a key aspect of genetic inquiry, shows great promise. By assessing a patient’s genetic framework, healthcare professionals can forecast how they may process psychotropic drugs. This tailored strategy can refine medication selection, reduce negative side effects, and improve treatment outcomes. While psychiatry hasn’t attained a point where medications can be flawlessly aligned with individuals based on genetic factors, ongoing studies continue to enhance personalized treatment methodologies.
## Pursuing Biological Markers in Psychiatry
In contrast to diabetes, where biomarkers such as blood glucose levels act as clear diagnostic and treatment indicators, psychiatry does not have universally recognized biological markers. However, advancements in this field are proceeding.
For instance:
– **Cortisol levels** have been associated with stress-related ailments like depression, anxiety, and post-traumatic stress disorder (PTSD).
– **Inflammatory indicators** are being explored for their involvement in mood disorders.
– **Neurotransmitter byproducts** and **hormonal discrepancies** offer insights into the biological basis of psychiatric conditions.
Although definitive diagnostic instruments derived from these observations are still forthcoming, the expanding comprehension of psychiatric biomarkers lays a solid groundwork for future precision psychiatry.
## The Role of Electrophysiology and Neurotechnology in Mental Health
Electrophysiological innovations are increasingly pertinent in psychiatry, aiding both diagnosis and therapy. A significant breakthrough is the adoption of AI-driven biofeedback, which the FDA has authorized for PTSD treatment.
Another innovative method is **transcranial magnetic stimulation (TMS)**. This non-invasive procedure is becoming recognized as an effective intervention for depression, anxiety, PTSD, and obsessive-compulsive disorder (OCD). By focusing on specific brain areas with magnetic impulses, TMS improves treatment results with minimal side effects.
An exciting advancement in neurotechnology is **Neuralink**, a brain-computer interface pioneered by Elon Musk. Still in the early experimental phase, this technology has the potential to revolutionize both the diagnosis and treatment of psychiatric disorders through direct brain interaction.
## The Influence of Artificial Intelligence (AI) in Psychiatry
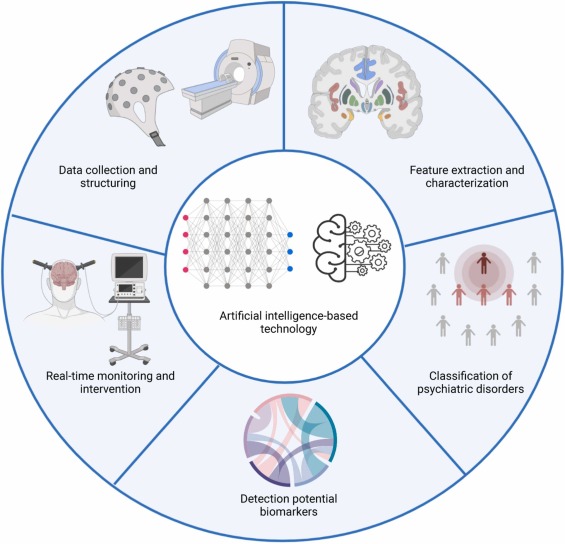
AI is reshaping psychiatry by improving diagnostic and therapeutic processes. AI-enhanced algorithms can evaluate facial expressions, speech patterns, and behaviors to identify early indicators of mental health issues.
For example:
– AI-assisted tools for **tardive dyskinesia** can recognize subtle movement irregularities with greater accuracy than human clinicians.
– AI-based vocal analysis is being investigated for its capacity to detect early signs of depression and other mental disorders by examining tone, speech rhythm, and vocabulary choices.
On the treatment front, AI has the ability to sift through extensive clinical data to assist psychiatrists in identifying the most suitable treatment approaches for individual patients. However, concerns regarding AI-induced inaccuracies, often termed “hallucinations,” highlight the necessity for human oversight to guarantee ethical and clinically reasonable decision-making.
## The Future of Psychiatry: Emphasizing Personalization and Prevention
The future of psychiat