Title: From Mechanical Aspirations to Medical Innovations: How Curiosity, Teamwork, and Project ECHO Influence the Future of Physician Education
Years ago, Dr. Daniel Johnson imagined a future in mechanical engineering. Engrossed in problem-solving, hands-on experiences, and case studies, he found fulfillment in uncovering the mechanics of the world—traits that ultimately steered him towards medicine. Upon discovering biomedical engineering, he redirected his ambitions towards medical school, where his innate curiosity and foundational learning would soon merge with practical patient care.
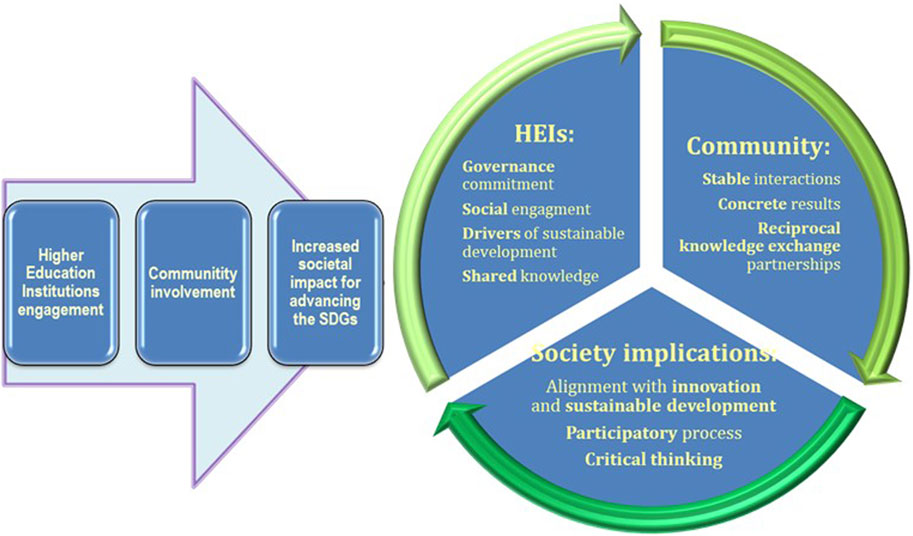
This life-altering journey has inspired Dr. Johnson to champion a vision for medicine that is more collaborative, driven by curiosity, and committed to continuous learning. Through personal anecdotes and forward-thinking concepts, his narrative highlights the significance of lifelong professional growth and introduces Project ECHO as an impactful remedy for the isolation and stagnation often experienced by clinicians.
The Medical Education Journey: A Base Craving Real-World Application
Like countless physicians, Dr. Johnson’s initial two years in medical school were abundant in didactic learning but lacked ties to actual patient interactions. It was only during his clinical years—third and fourth years of medical education, alongside his residency—that the foundations of true comprehension and enthusiasm began to flourish.
Suddenly, education evolved beyond theory; it became hands-on. Classrooms shifted to busy hospital rounds—lively environments where medical knowledge converged with critical thinking in live patient interactions. These instances rekindled his engineering mindset. Medicine transcended rote learning—it transformed into applied science, collaboratively constructed within a team framework.
Two Scenarios, Two Insights
Dr. Johnson reminisces about two crucial cases from his medical training that influenced his approach to patient care. During the onset of the AIDS crisis—then unrecognized and referred to as Gay-Related Immune Deficiency—he and a medical team confronted a patient suffering from an unexplained pneumonia. An investigation through medical literature turned up a fresh report of related cases in California. Equipped with newly found insights, the team developed a treatment plan that ultimately saved the patient’s life.
In a separate scenario, an elderly woman presented neurological symptoms deemed “inexplicable.” However, Dr. Johnson, having recently participated in a lecture on sexually transmitted infections, decided to take a sexual history—an approach that was then considered unconventional. She disclosed a long-dormant exposure to syphilis, which resolved the mystery. Application of long-standing knowledge at the opportune moment transformed her medical prognosis.
From these moments, Dr. Johnson gleaned vital lessons:
1. Timely Knowledge is Crucial: Effective care depends not just on existing knowledge but on the capacity to continually uncover, access, and utilize new insights.
2. Curiosity and Willingness to Explore are Imperative: His readiness to challenge norms and pose “difficult” questions, even as a student, uncovered diagnoses overlooked by others.
The Challenge of Sustaining Curiosity
Fueled by his formative years of engagement and exploration, Dr. Johnson quickly recognized that post-residency and fellowship, physicians often became disconnected from vibrant, collaborative learning. Daily activities turned fragmented. Physicians found themselves overwhelmed, at times isolated, and deprived of the collaborative problem-solving that had previously invigorated their practice.
Nevertheless, the urge to learn, connect, and grow is never truly extinguished—it merely requires a framework to nurture it. That’s where Project ECHO steps in.
Project ECHO: A Revolutionary Shift in Medical Learning
Project ECHO (Extension for Community Healthcare Outcomes) is a groundbreaking model that redefines conventional medical training by empowering clinicians at all levels to both teach and learn from one another. Originating at the University of New Mexico to combat a gap in hepatitis C expertise, the model has expanded into a global network promoting education across various health concerns.
ECHO programs operate like virtual “hospital rounds”—but in a democratized way. Sessions are open, free, and tailored for community-focused care. They commence with a brief lecture by a specialist followed by a case presentation by a participant. What ensues is a collaborative dialogue that leverages the expertise of all participants, culminating in actionable insights for immediate patient care.
This “all teach, all learn” approach not only encourages knowledge sharing, but also fosters professional camaraderie and mutual support—elements frequently lacking in contemporary clinical practice.
Where ECHO Excels: Authentic Stories and Tangible Impact
At the University of Chicago, Dr. Johnson played a key role in establishing one of the first ECHO Superhubs globally. Through more than twenty ECHO series each year, his team facilitates educational efforts on a range of topics, including childhood obesity, hypertension, opioid dependency, and mental health.
The results have been transformative. One pediatrician involved in the obesity series finally witnessed meaningful improvements in patient outcomes after years of struggle. Residents from under-resourced community hospitals gained confidence and proficiency in managing ADHD cases. A physician in Washington state even included ECHO participation in his contract—demonstrating its importance in everyday practice.
The Significance of ECHO in Medical Education
What if this paradigm were adopted earlier in training? Dr. Johnson envisions ECHO