Title: What Has Led to the Lowest Faith in Government Health Entities? Heightened Conflicts of Interest
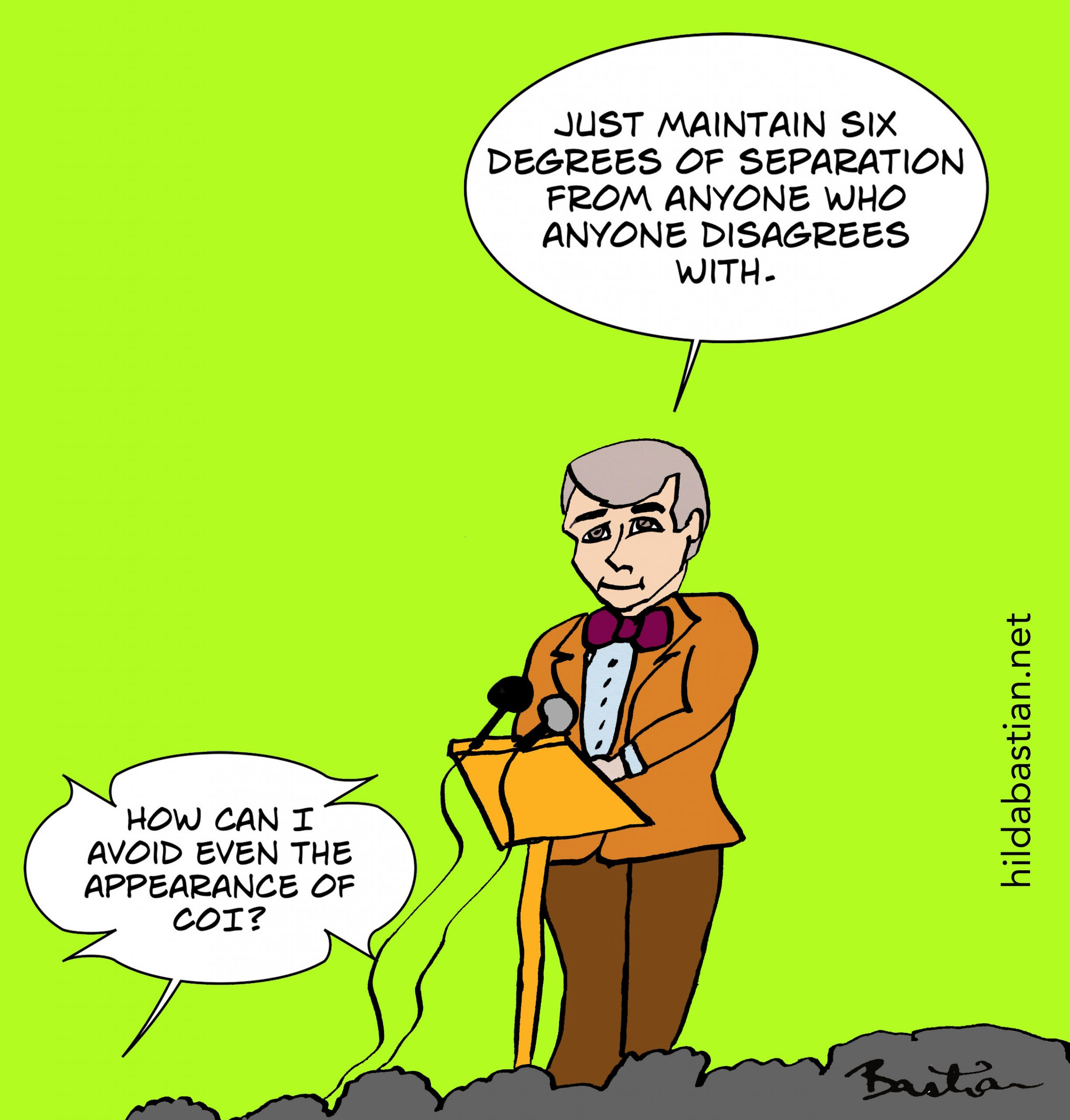
Trust in U.S. government health organizations such as the Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) has plummeted to unprecedented levels—and many see the reasons for this decline as clear. Increasing worries surrounding conflicts of interest (COIs) among leading regulators and the extensive influence of pharmaceutical companies have contributed to a waning confidence in agencies once regarded as cornerstones of public health.
While skepticism toward the pharmaceutical sector is not a recent phenomenon, the escalating intertwining of industry and regulators brings new doubts about the objectivity of choices that impact countless lives.
The Origins of Distrust: FDA and the User Fee Era
A significant change took place with the FDA’s implementation of the Prescription Drug User Fee Act (PDUFA) in 1992. The intention of the Act was to expedite drug approvals by permitting drug manufacturers to pay fees to support agency functions. While this sped up the review process, critics argue it paved the way for excessive influence.
This funding approach has created a dilemma: the FDA increasingly depends on funding from the very companies it is supposed to oversee. In certain years, user fees even surpass congressional appropriations, leading critics to fear the agency is becoming overly aligned with industry interests.
Concerns Over Trial Integrity
Another critical issue is the rising number of industry-sponsored clinical trials. It has become commonplace for pharmaceutical companies to fund studies on their own products, which are then heavily referenced in regulatory submissions, medical literature, and popular media.
The risk for bias in these trials is substantial. Positive outcomes can be highlighted, while adverse results may be minimized or ignored. Detractors question: how frequently would a company support and release studies that challenge its products?
For instance, consider current research on GLP-1 drugs—a type of diabetes medication repurposed for weight loss—where virtually all prominent studies showcasing their advantages are funded by their manufacturers.
The FDA’s Revolving Door
The pattern of industry connections among FDA leaders has only heightened further distrust.
Dr. Scott Gottlieb, who served as FDA Commissioner from 2017 to 2019, had a multitude of prior ties to the pharmaceutical sector, including consulting roles and board memberships. Upon leaving, he returned to the private sector, joining Pfizer’s board.
Dr. Robert Califf, who held positions in both the Obama and Biden administrations, was even more deeply involved in the industry. He openly supported cooperation with drug manufacturers, even amid personal connections that raised eyebrows within the healthcare community.
Before them, Dr. Margaret Hamburg resigned amid ethical concerns. Ironically, despite her earlier warnings about widespread COIs, she later found herself named in lawsuits involving conflict accusations.
The CDC’s Conflicting Allegiances
Less known to the public is the CDC Foundation, a legally independent yet closely connected nonprofit formed in 1992 to promote private-sector donations and collaborations. Although aimed at funding vital projects, its acceptance of contributions from corporations including Coca-Cola, Bayer, and 3M has raised alarms.
The 2017 appointment of Dr. Brenda Fitzgerald as CDC Director sparked controversy following revelations of her acceptance of Coca-Cola funding while serving as Georgia’s health commissioner. The company, infamous for its association with sugary beverage consumption, sought to shape narratives around obesity and physical activity during her time in office.
Fitzgerald resigned after only six months when it was revealed that she had invested in tobacco stocks while leading the nation’s foremost public health agency.
Regulatory Capture and Media Inaction
The revolving door phenomenon—that is, the transfer of personnel between public positions and the sectors they regulate—has long affected both the FDA and CDC.
Former CDC Director Dr. Julie Gerberding, who oversaw significant flu vaccine initiatives during her term, became the head of Merck Vaccines directly after leaving her post—raising concerns about potential regulatory leniency.
Meanwhile, mainstream media coverage of these COIs tends to be subdued, likely due to conflicting interests. With television networks increasingly reliant on pharmaceutical advertising revenue, critics argue that editorial independence could be at risk.
Furthermore, scientific journals that once banned industry-sponsored research have adjusted their guidelines. Some observers speculate that they are accommodating Big Pharma in a bid to recover lost advertising revenue.
Capitol Hill Influence: Pharma’s Extensive Reach
The influence of the pharmaceutical industry extends well beyond health agencies and into Capitol Hill. In 2020 alone, over two-thirds of U.S. lawmakers received campaign donations from drug companies. Reportedly, there are three pharmaceutical lobbyists for each member of Congress.
Such influence obstructs the possibility of meaningful legislative changes, from drug pricing transparency to enhanced post-market monitoring of expensive therapies.
Why This Matters for Public Health
The consequences of entrenched COIs go well beyond regulatory credibility—they directly impact patient trust, medical decision-making, and public health results.
When government agencies endorse vaccines, new medications, or health recommendations, the public must trust that those endorsements are based solely on scientific evidence and safety, not financial gain. Failures to uphold strong conflict-of-interest regulations endanger that trust.