Title: Grasping the Increase in Adult Female ADHD Diagnoses: Obstacles, Hormones, and Optimism
By Arti Lal, MD
In recent times, the perception of Attention-Deficit/Hyperactivity Disorder (ADHD) has significantly evolved. Once predominantly recognized as a diagnosis for hyperactive young boys, ADHD is now gaining traction among women — especially adult women. From 2020 to 2022, adult female diagnoses nearly doubled, driven by heightened awareness and shifting societal narratives that have prompted more women to seek evaluations for previously unaddressed symptoms.
Despite this rise in diagnoses indicating a step forward, many challenges persist. Both clinicians and patients must navigate a mental health system that is still adapting to the complexities and subtleties of ADHD as it presents in women.
Breaking the Stereotype
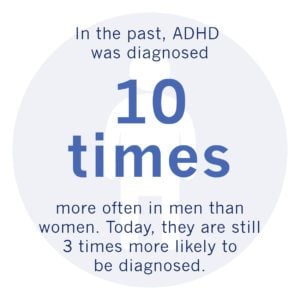
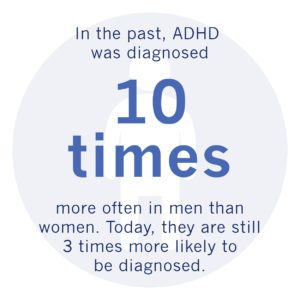
For years, ADHD was almost solely linked to young boys who faced challenges in school due to impulsivity and hyperactivity. This limited perspective resulted in girls — and subsequently adult women — being frequently underdiagnosed. Numerous women concealed their symptoms, internalized their difficulties, or were misdiagnosed with depression or anxiety.
Today, with the support of online communities, discussions on social media, and advocacy initiatives, many women are coming to terms with the idea that struggles with concentration, forgetfulness, emotional instability, and chronic disorganization are not personal shortcomings but possible indicators of neurodivergence.
The Diagnostic Discrepancy
Obtaining an accurate diagnosis is often the first and most daunting hurdle. Studies reveal that enduring gender biases can obstruct the diagnostic journey. Healthcare providers may overlook signs in women or completely neglect their concerns. Indeed, almost one-third of women in the 2022 KFF Women’s Health Survey felt dismissed by their healthcare practitioners when expressing health-related issues, a trend that also permeates mental and behavioral health evaluations.
Even when women secure an assessment, they encounter additional challenges. A significant obstacle is the way symptoms present: women frequently exhibit “inattentive” ADHD, which is less conspicuous than the “hyperactive-impulsive” variant. Hyperactivity in women may manifest differently — often seen as internal restlessness, racing thoughts, or excessive speech — yet can be equally debilitating.
To further complicate matters, ADHD often overlaps with anxiety and depression. These co-occurring conditions, which are more prevalent in women, can obscure ADHD signs or be wrongly classified as primary diagnoses. Without appropriate tools and well-informed evaluations, healthcare providers risk overlooking or misclassifying signs of ADHD.
Objective Assessment and Tackling Bias
Conventional ADHD evaluations predominantly depend on subjective self-reports, childhood histories, and feedback from observers — all of which can be particularly unreliable for adult women. Memories can fade, records might be lost, and symptoms may have gone unnoticed for years as they did not align with the “classic” ADHD profile.
To counter this, numerous practices are adopting objective assessment tools that yield biometric data. These evaluations measure attention, activity, and impulsivity in real time, providing a critical layer of precision to clinical observations. Objective data can assist in distinguishing ADHD from similar conditions and affirm the experiences of women who often attribute their challenges to personal failings.
The Hormonal Element
Even with a correct diagnosis, managing ADHD symptoms in women is complicated by a factor often neglected in research and treatment methodologies: hormones. Estrogen and progesterone markedly influence how ADHD symptoms manifest and the efficacy of medications.
Estrogen, for instance, is believed to exert a protective effect, enhancing cognitive abilities such as focus and working memory. As estrogen levels fluctuate throughout the menstrual cycle, during perimenopause, or menopause, women can experience noticeable variations in symptom intensity. For many, the week or two leading up to menstruation — when estrogen levels decrease and progesterone rises — proves particularly challenging.
Research indicates that women with ADHD are more prone to experiencing Premenstrual Dysphoric Disorder (PMDD), characterized by severe mood swings, irritability, and even suicidal ideation. Some women resort to modifying their medication doses to self-manage, a tactic that carries risks without medical oversight.
Hormonal changes also significantly impact key life transitions. Adolescents, expectant mothers, and those approaching menopause often report shifts in symptom patterns, yet providers may fail to link these changes to their ADHD. This issue is further compounded by the lack of comprehensive studies on the safety and effectiveness of ADHD medications during pregnancy and other hormone-sensitive periods.
A Call for Comprehensive, Data-Informed Care
Given these complexities, a uniform approach to ADHD treatment falls short — especially for women. By utilizing objective measurement tools and screening procedures that acknowledge hormonally influenced symptom changes, healthcare providers can offer more tailored and effective care.
For example, by tracking symptoms throughout different phases of a patient’s menstrual cycle, clinicians can identify trends and modify medication plans accordingly. Evidence-based adjustments can be made to assist patients during their most symptomatic periods, ultimately enhancing both quality of life and health outcomes. These tools also help validate patients, allowing them to see concrete data that supports their experiences.