Veterans merit the finest health care that our country can provide, yet honoring this commitment frequently demands overcoming significant obstacles. Approximately 9 million veterans obtain care through the VA, with one-third residing in remote areas far from VA facilities. Addressing their needs necessitates innovative strategies that merge expertise, technology, and strategic collaborations.
## Why VA’s Holistic Model Surpasses Conventional Care
The VA distinguishes itself with its cohesive, long-term care strategy. Unlike the disjointed experiences many Americans endure—navigating among providers who rarely communicate—veterans benefit from a health care system that monitors their needs from military discharge to end-of-life care.
As an executive advisor to four VA secretaries across two administrations, I personally witnessed how veterans gain from care that is driven by data, emphasizes prevention, and concentrates on results. Most Americans would envy this level of integration. In the private sector, patients frequently manage multiple specialists—general practitioners, surgeons, gynecologists, cardiologists—who seldom share information or synchronize treatments.
This integration has empowered the VA to cultivate exceptional expertise in conditions that disproportionately impact veterans, such as traumatic brain injury (TBI), combat-related mental health challenges, and cancer treatments. VA centers of excellence are so esteemed that families of non-veterans sometimes seek access to this superior care. I recall instances where parents of teenagers who endured TBIs in vehicle accidents inquired whether the VA could assist—because the VA’s expertise clearly eclipsed what was accessible in many private care environments.
## When Enhanced Access Encounters Disjointed Systems
The 2018 MISSION Act marked a pivotal change—broadening veterans’ access to community care when faced with prolonged wait times or residing too far from VA facilities. However, with this opportunity arose a challenge: maneuvering the fragmented health care landscape where numerous providers lacked the proficiency to handle military-specific conditions.
To facilitate this transition, the VA established the Community Care Network (CCN), linking eligible veterans with community providers according to specific criteria. The aim: More choices and enhanced access to timely, high-quality care closer to home.
Nonetheless, private-sector providers suddenly encountered patients with distinct physical traumas and mental health requirements they were not equipped to address. Veterans entering these systems anticipate their care teams to comprehend military culture and service-related concerns. All too frequently, that expectation remains unfulfilled.
## The Administrative Labyrinth of Claims Processing
Behind the scenes, another hurdle prevails: Claims processing. VA claims differ fundamentally from conventional insurance, necessitating specialized knowledge.
The VA’s established EMR system, VistA, predates most commercial systems and contains decades of invaluable longitudinal data. Processing claims from this system with community providers entails navigating intricate coding, reimbursement regulations, and documentation standards.
To tackle these issues, the VA is advancing toward the Oracle Cerner-based Federal Electronic Health Record (EHR), improving interoperability amongst the VA, Department of Defense (DoD), and CCN providers. By standardizing records, this system will enhance coordinated, data-driven care—regardless of where a veteran receives treatment.
Yet, even as platforms like Cerner and Epic facilitate clinical data sharing, administrative difficulties remain. Inconsistent data standards, fragmented provider networks, and variable documentation continue to delay processes and lead to under-reimbursement. Hospitals collect only about 70 percent of what they are owed on VA claims, writing off the remainder and jeopardizing long-term access to care for veterans.
## Human + Machine: The Future of Claims and Care
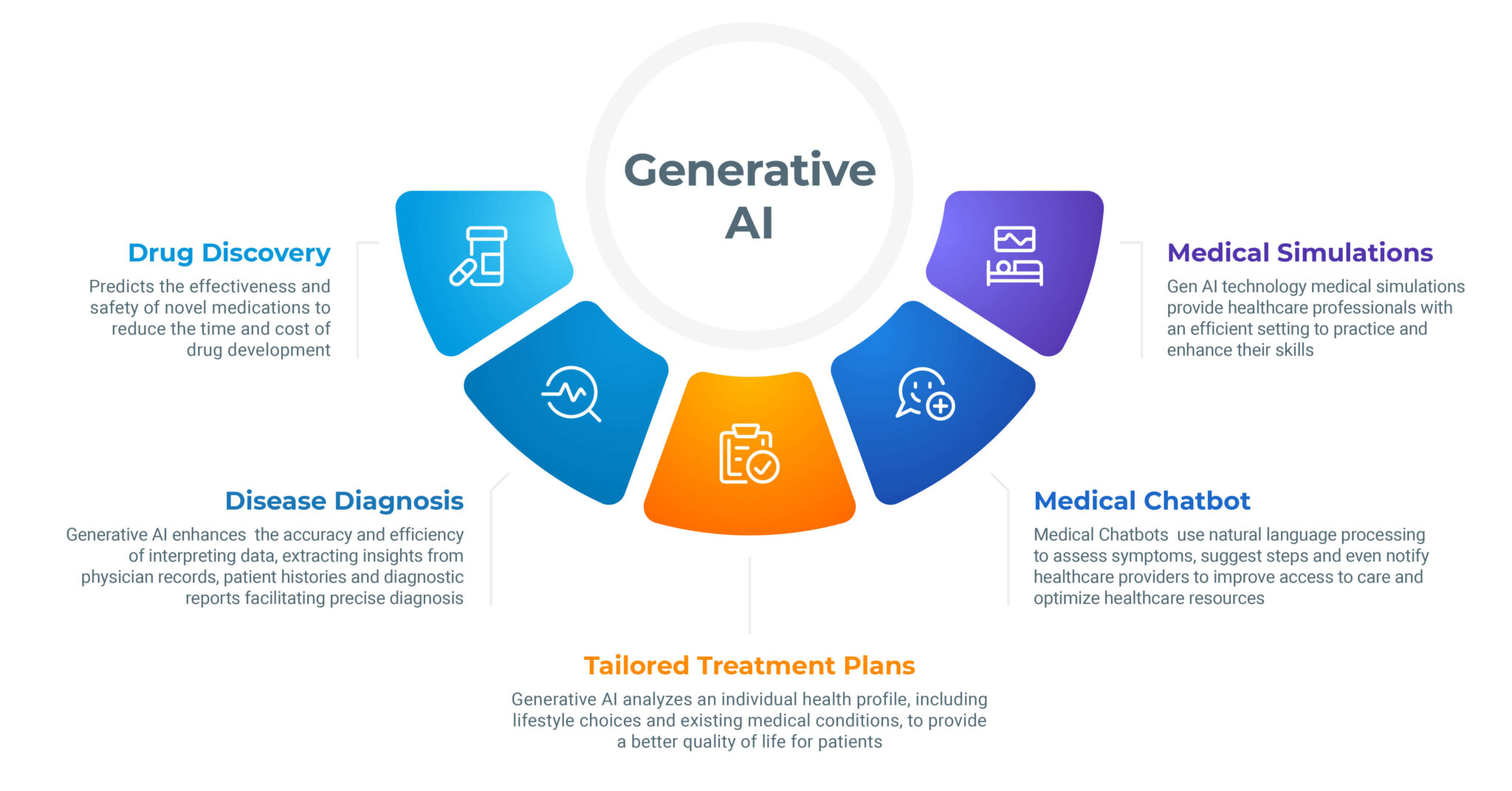
Technology alone will not resolve these challenges. The way forward lies in merging intelligent systems with profound domain expertise. Artificial intelligence can assist, but only when it comprehends the context.
This is the potential of Context-Augmented Generation (CAG), a burgeoning concept where AI tools are trained on specialized datasets to interpret claims and care documentation with greater accuracy. In the context of the VA, integrating this technology with expert human oversight guarantees fair reimbursement for providers and ensures veterans receive the care they need.
## Transforming Shared Missions into Movements
Addressing veteran health care challenges frequently requires unconventional partnerships. In developing public-private collaborations, I have discovered that success begins with one crucial inquiry: Who else is invested in this?
When two organizations align on a primary strategic objective, collaboration thrives. However, when priorities diverge, even the best ideas may stumble. Especially in government partnerships, comprehending regulatory and institutional limitations is essential. Roles and responsibilities are often defined by Congress, hindering flexibility. Yet when framed around the common goal of enhancing veteran care, many are motivated to act.
A compelling instance arose during the COVID-19 pandemic. The VA confronted a severe PPE shortage. I contacted inventor Dean Kamen, who leveraged his global supply chain to procure vital equipment. Despite skepticism about whether a single entrepreneur could assist a federal agency, our partnership delivered nearly 25 planeloads of masks, gowns, and gloves to VA facilities across the country.
## Broadening Access Through Technology and Collaboration
Technology will persist in transforming veteran care, particularly for rural communities. The VA was a forerunner in telehealth long before the pandemic.