I suffered a stroke at the age of five. It was an ischemic incident, uncommon in children, challenging to diagnose, and frequently overlooked in its early phases. I faced a sudden decline in motor capabilities that resulted in an extensive rehabilitation journey. I dedicated months to relearning how to walk, maintain balance, and execute fundamental movements, under the guidance of physical therapists and the consistent framework of routine. I was too young to comprehend what had transpired, but I understood it had altered something significant. That ordeal, albeit challenging, influenced my perspective on recovery and the brain’s capacity to adapt.
Years later, discovering vagus nerve stimulation, or VNS, offered a fresh viewpoint on the potential for stroke survivors today. The notion that a specific neural pathway could be utilized to encourage plasticity and improve functional recovery highlights significant advancements in the treatment of neurological injuries.
**From epilepsy to stroke rehabilitation**
Vagus nerve stimulation was initially authorized by the FDA in 1997 for epilepsy that did not respond to treatment. It gained further approval in 2005 for depression that was resistant to treatment. Gradually, researchers started exploring if the same technology could be applied to conditions with motor deficits, including stroke.
Early experiments in animal models revealed that combining VNS with physical movement enhanced plasticity in the motor cortex. These discoveries established the foundation for human trials that investigated whether synchronized stimulation of the vagus nerve could bolster the brain’s relearning of motor skills that were lost.
In 2021, a crucial multicenter clinical trial known as VNS-REHAB was published in The Lancet. This study involved individuals who had chronic ischemic strokes and upper limb difficulties. The results indicated that patients who received VNS alongside rehabilitation activities exhibited considerably greater enhancements in motor function compared to those who underwent therapy alone. These improvements translated into a better performance of daily tasks, including grasping, lifting, and handling objects.
Later that same year, the FDA approved VNS for rehabilitation following a stroke, making it the first neuromodulation device sanctioned specifically to aid motor recovery post-stroke.
**Expanding the timeline for recovery**
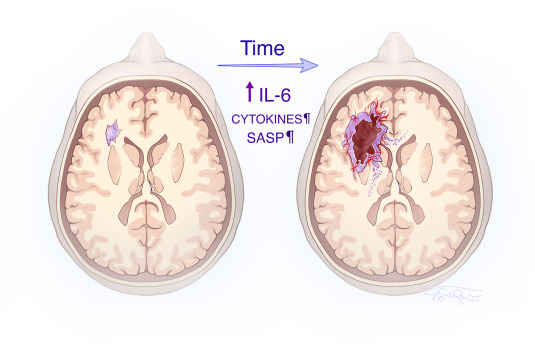
Traditionally, stroke recovery has been perceived as most effective during the initial months after an injury. After that timeframe, patients are often advised to modify their expectations. The incorporation of VNS into stroke rehabilitation questions that timeline.
By activating the vagus nerve during motor activities, the therapy enhances the brain’s ability to detect and consolidate that movement. This mechanism aids in reorganizing damaged motor circuits, even well after the initial injury. For numerous patients, this implies that functional improvements are attainable long after what conventional recovery frameworks propose.
Instead of substituting rehabilitation, VNS amplifies it. This integration symbolizes a transformation in mindset. Stroke recovery is no longer confined to a limited timeframe but can evolve into an ongoing, flexible process, backed by technology that collaborates with the brain’s inherent plasticity.
**Barriers to broader use**
Despite VNS being FDA-approved and supported by clinical studies, access is still limited. The procedure necessitates the implantation of a pulse generator and consistent alignment with physical therapy sessions. This requirement for specialized apparatus and training may hinder widespread application, particularly in smaller or underfunded rehabilitation facilities.
Insurance coverage also presents an obstacle. Like many novel treatments, VNS has yet to gain universal acceptance among payers. This fiscal ambiguity creates further challenges for both patients and providers. Furthermore, awareness is relatively low. Numerous clinicians, patients, and caregivers remain unfamiliar with the therapy and its prospective advantages.
Addressing these challenges will necessitate enhanced education, funding for training initiatives, and policy modifications to facilitate reimbursement. As more clinicians witness the advantages and more patients relay success stories, adoption is likely to rise.
**A broader shift in neurorehabilitation**
Vagus nerve stimulation is a component of a broader evolution in stroke treatment. Technologies such as transcranial magnetic stimulation, robotic-assisted therapy, and brain-computer interfaces are also transforming how clinicians approach recovery. These innovations prioritize targeted, data-driven interventions that promote sustained function and autonomy.
As research advances, forthcoming studies will refine the application of VNS, determine which patient demographics gain the most benefit, and investigate new uses beyond stroke. Ongoing investment in this area is crucial. Stroke continues to be a primary cause of adult disability, and the demand for effective rehabilitation tools is steadily increasing.
Patients who undergo a stroke frequently encounter a prolonged and challenging recovery journey. Every incremental improvement in function can signify increased independence and a better quality of life. Tools like vagus nerve stimulation equip clinicians with innovative methods to assist patients in achieving those objectives.
*William J. Bannon IV is a premedical student.*