Significant attention has been directed towards the initiative by President Donald Trump and the pharmaceutical sector to provide direct-purchase drug programs at substantially reduced prices. Following the unveiling of these new initiatives and TrumpRx, we’ve encountered news and opinion articles from every major source, yet absent from this dialogue is one of the most crucial perspectives: that of the patient. Essential inquiries remain unresolved:
“What implications does this have for my treatment?”
“Will this integrate with insurance?”
“Why are the prices so much lower?”
The partnership and innovative thinking surrounding new direct-purchase drug programs is a promising advancement for the 8 million individuals in the U.S. living with psoriatic disease, myself included. These measures indicate a readiness to investigate the collaborative, novel strategies necessary to decrease the cost of prescription medications. After years of disappointing inaction, fresh ideas and new strategies are welcomed and encouraged for those dealing with chronic illness.
Nevertheless, the worry is that this may turn out to be yet another isolated solution that only addresses a tiny aspect of a healthcare system needing comprehensive reform. While some question or debate the viability, safety, and affordability of direct-to-consumer drug purchasing, there are established, bipartisan healthcare solutions primed for implementation today.
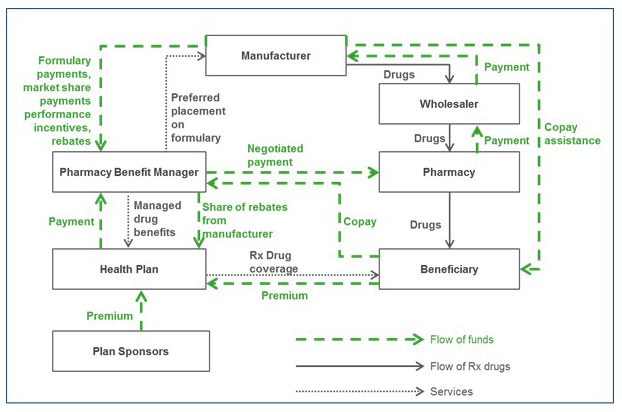
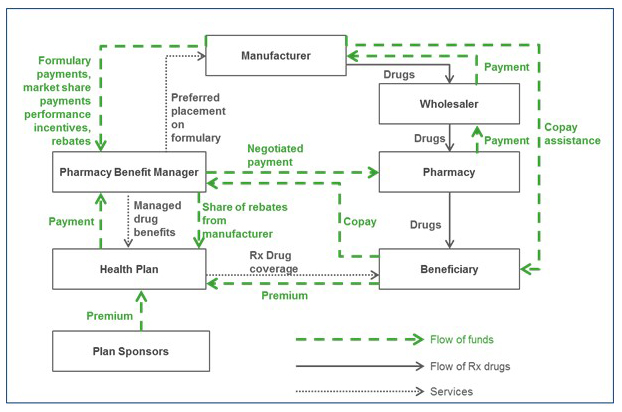
At present, we confront a healthcare framework that rewards and incentivizes elevated costs, meaning that if you fall ill, you and your family bear more expenses to keep other people’s premiums lower. Significant pharmacy benefit manager (PBM) reform will bring clarity and responsibility to our healthcare system. Moreover, any PBM reform must encompass the most practical and patient-focused change to date: altering the practice of step therapy.
The bipartisan-supported Safe Step Act has been introduced in both legislative chambers and is awaiting Congress’s return.
We cannot afford to spend more time prolonging the cycle of healthcare solutions “whack-a-mole” that Americans have been trapped in for decades. Our community (all communities) deserves better. All Americans should have access to a healthcare system that prioritizes healthier lives without exploiting the ill to subsidize the costs for others.
PBM reform and the Safe Step Act symbolize two sensible, sustainable, systemic solutions that can assist in providing Americans with the healthcare they require at prices that won’t devastate their finances. Since the Safe Step Act was initially presented in 2017, over a dozen patient advocacy groups including the National Psoriasis Foundation, the Arthritis Foundation, the Crohn’s and Colitis Foundation, the National Alliance on Mental Illness, and others have taken the lead in advocating for progressive policy changes necessary to promote systemic transformation.
Innovative solutions to high consumer costs for prescription medications should be applauded. However, let’s not allow that to distract us from the bipartisan legislative remedies that have been in the pipeline for years. We can (and should) pursue both pathways.
The question at hand is straightforward: Will we be able to rejoice in this significant accomplishment that defies the trend of “divided times”, or will we squander yet another chance to enhance the lives of Americans by neglecting to tackle what we all acknowledge is a substantial issue?
Leah M. Howard serves as the president and chief executive officer of the National Psoriasis Foundation (NPF). She is an attorney and advocate for patient rights, leading the world’s largest nonprofit organization focused on psoriatic disease support and research. The NPF advocates for over eight million individuals in the United States living with psoriasis and psoriatic arthritis, united by the vision of creating a world devoid of the challenges posed by psoriatic disease.
Leah has lived with psoriasis for twenty-one years and possesses over two decades of experience collaborating with national health and disability organizations, local governments, and prominent healthcare and research institutions. She believes that addressing today’s healthcare challenges begins with engaging those living with chronic conditions, such as psoriasis and psoriatic arthritis. In the past decade, Leah has empowered individuals with psoriatic disease to communicate their challenges to policymakers at both the state and federal levels, as well as to regulators and health agency leaders. This advocacy has led to numerous advancements for the community, including over forty new state laws that enhance access to treatment.
Leah has established the NPF as a pivotal voice in efforts to evaluate value and reflect patient preferences in health outcomes. She has also initiated efforts to involve non-traditional patient-advocacy associates, such as health insurers, pharmacy benefit managers, and employers, starting with the NPF Payer Roundtable series launched in 2016. Under Leah’s guidance, the NPF has made it a priority to serve all segments of the community. Currently, the foundation engages with over 2.75 million individuals annually through its highly accessible website.