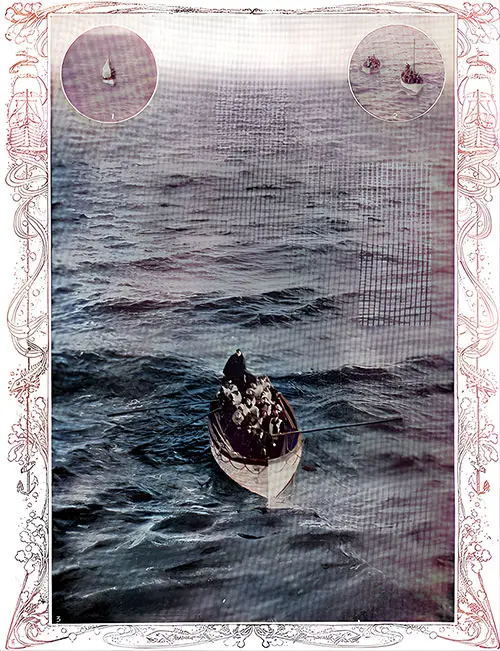
Two years prior, Drs. Aaron Morgenstein, Corinne Sundar Rao, and Shreekant Vasudhev established a striking analogy between the ill-fated journey of the Titanic and the impending crisis in U.S. health care. They pointed out deep-rooted problems such as administrative hubris, antiquated methodologies, and inadequate resources, cautioning that without considerable adjustments, the health care system was steering toward a calamity.
Now, in 2025, the iceberg has collided, and the fractures are expanding. The Titanic didn’t go down just because it struck an iceberg. It sank due to a lethal mixture of obsolete systems, overconfidence at the helm, and a refusal to adjust course despite numerous alerts. Unfortunately, the field of medicine is encountering a similar demise.
Obsolete procedures: disregarding the modern tempest
Similar to how the Titanic depended on outdated ship models and insufficient lifeboat provisions, the current health care system clings to obsolete processes that fail to benefit either caregivers or patients. Electronic health records were meant to enhance efficiency but have instead buried doctors under a heap of clicks and trivial tasks. Paperwork has supplanted patient engagement. The vessel is burdened by red tape while genuine innovation (such as direct physician-patient frameworks) struggles to keep from sinking.
Administrative excess: too many leaders, too few lifeboats
The Titanic lacked enough lifeboats for its passengers; contemporary health care is burdened with an excess of administrators for its dwindling number of doctors. Non-clinical roles keep multiplying while those delivering care are stretched thinner than ever. Physicians are now dedicating more time to justifying care to insurers than to delivering it, combating denial after denial, advocating for essential treatments, and witnessing as outsiders undermine their medical judgment.
Employment over independence: when the team is bound
On the Titanic, the crew had limited power to challenge disastrous actions. Today’s physicians are facing a similar decline in autonomy. Increasingly funneled into employment frameworks, they are urged to prioritize corporate metrics over clinical insights. The autonomous physician is becoming a rare entity, with progressively fewer granted the ability to practice medicine on their own terms. The crew’s freedom has been purchased, and with it, the essence of the profession.
Burnout, migration, and premature retirement: when the crew flees
Confronted with dwindling Medicare reimbursements, endless claim denials, mounting documentation pressures, and the stifling of their professional freedom, numerous physicians are making the tough decision: exit medicine entirely. Burnout rates are at an unprecedented high. Physicians are retiring early, changing professions, or stepping back from clinical roles, not because they wish to forsake patients, but because the system has forsaken them. The vessel is sinking not due to the frailty of the passengers, but because the foundation they relied upon has decayed.
Falling Medicare reimbursements: operating the ship on empty
Amid rising inflation affecting every aspect of life, Medicare reimbursements for physicians continue to diminish in real value. As costs climb and demands intensify, compensation dwindles. It’s analogous to the Titanic’s operators asking the crew to toil harder, in harsher conditions, with reduced provisions, and expecting improved results.
Two years on: what has transformed
In reality, very little. Awareness has increased, but authentic reform is still out of reach. Much like the Titanic’s captain disregarding iceberg alerts, health care leadership persists in fixing fractures with empty promises instead of steering toward safety. Physicians, once the unsinkable driving force behind patient care, are increasingly finding themselves confined below deck. If the situation remains unchanged, the downfall will not be abrupt; it will be a gradual, relentless decline into mediocrity, where fewer physicians care for more patients, under deteriorating conditions, for diminishing rewards.
There remains a slim opportunity to alter the trajectory. But only if doctors reclaim their voice, insist on a position at the helm, and reconstruct medicine with the patient-physician rapport (not the insurer or administrator) as its foundation. Otherwise, history will reflect on this period and ponder how we failed to heed the lessons of the Titanic until it was far too late. And just as Jack reminded Rose in the frigid waters, a note to physicians and patients alike: “You jump, I jump, remember?” We are still in this together, but time is diminishing to rescue us both.
Corinne Rao is a physician specializing in internal medicine, practicing as an independent contractor at various health care facilities, the proprietor of an internal medicine practice, and a member of FlexMedstaff. In her leisure time, she enjoys ballroom dancing.
Shreekant Vasudhev is a physician specializing in internal medicine.
Aaron Morgenstein is an orthopedic surgeon.