**The Elephant in the Room: The Blind Men, Pain Management, and an Unseen Crisis**
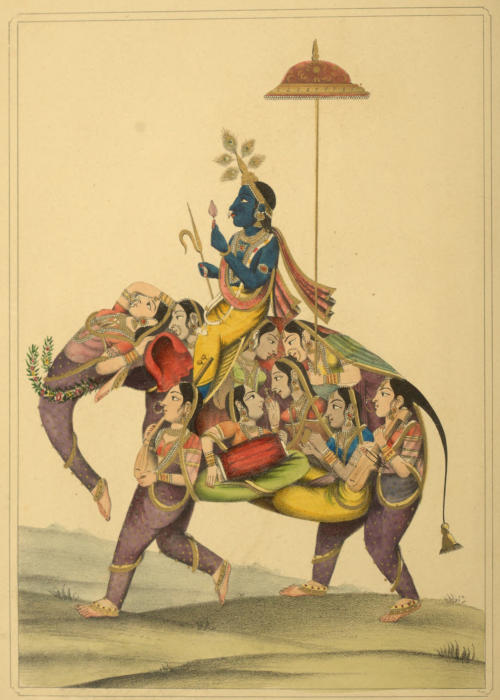
The tale of the blind men and the elephant is an age-old parable rooted in ancient Indian and Buddhist lore. It narrates how various blind men each come into contact with a distinct part of an elephant, thus forming highly differing views of what the elephant truly resembles. This allegorical story mirrors the fragmented perspectives prevalent in today’s pain management sector—a domain where the excessive specialization of health care providers risks overshadowing a comprehensive understanding of patient care, particularly with regards to chronic pain and opioid consumption.
In the evolution of medical frameworks addressing pain, two predominant paradigms surface: the psychological and the physiological. Sigmund Freud and Carl Jung in the early 20th century suggested that pain was largely connected to the mind, indicating that modifying a patient’s mental condition could alleviate pain sensations. Fast forward to 1980, when the DSM-III distinctly classified pain as a possible brain disorder, paving the way for a medication-focused treatment approach—a trajectory that has since been adopted by the broader medical community.
Yet, the pharmaceutical drive of the 1990s, which identified pain as the “fifth vital sign” and advocated for opioid use, has seen a decline. Following a surge in opioid prescriptions, culminating in the early 2000s with pill mills, regulators adjusted the course by labeling opioids as dangerously over-prescribed. New guidance from the CDC, initially rolled out in 2016 and updated in 2023, encourages health care providers to prioritize non-drug interventions, albeit lacking substantial alternative evidence when compared to pharmaceutical treatments.
At the center of this dilemma lies the patient—frequently overlooked and poorly treated. With one in four American adults experiencing daily pain, twenty-five million confront pain so severe it hampers daily functions. Regrettably, healthcare policies and insurance frameworks, in many instances, create obstacles for these patients seeking the essential care they desperately require, often favoring costly treatments over economically viable opioids without adequate evidence showcasing their superiority.
Despite the urgent need for interdisciplinary approaches and transparent communication across medical domains, a prevalence of biases intertwined with policy choices clouds sound decision-making. Thus, while lawmakers and healthcare providers enact guidelines that leave numerous patients without care, the credibility and effectiveness of extensive chronic pain management diminish. In the meantime, alternative pain management solutions tend to be exorbitantly priced and minimally beneficial, resulting in increased patient distress and financial burden.
The groundbreaking insights of the late Ron Melzack into pain science highlight the necessity of considering both the mind and the brain concurrently. Melzack dispelled popular misconceptions regarding morphine-related addiction, arguing that when used appropriately for pain management, addiction is significantly less common than traditional narratives indicate. Recent studies revealing genetic connections to addiction and opioid processing lend support to this perspective, advocating for more tailored, individualized treatment strategies.
However, the urgent message remains overshadowed in formal prescribing directives, resonating themes of inadequacy and exclusion that fail to safeguard physicians and patients from legal repercussions, addiction, or outright negligence. As healthcare providers, researchers, and policymakers fervently advocate against governmental interference in scientific methodology, the demand intensifies for rational, evidence-based reform to combat the epidemic of opioid denial and unfounded accusations targeting healthcare professionals.
In what resembles a whirlwind of medical confusion, specialists debate symptom-focused frameworks, oblivious to the crisis reflected in unmet patient demands. The moment has arrived to confront the elephant in the room, contemplate Hippocrates’ adage of “Do No Harm,” and endeavor toward a holistic, compassionate strategy for managing pain—recognizing and deriving insights from every viewpoint, whether blind or not.