With the arrival of the fall and winter seasons, my clinic in the Bronx prepares for an influx of anxious parents. A toddler presenting with itchy, watery eyes and a runny nose has become a distressingly frequent occurrence. Parents discuss their struggles with poorly ventilated homes, mold growth, and roach infestations, coupled with housing instability; in addition, the dangers of RSV, flu, and COVID-19 in daycare and schools aggravate congestion and lead to frequent emergency room visits.
With demanding responsibilities requiring their attention, rushing to get their child tested with an allergy panel at the first indication of a sneeze might appear to be the most appropriate choice. This instinct is justifiable. However, in many areas of pediatric care, allergy panels increase unnecessary expenses and result in parents dealing with perplexing outcomes.
In my view, we require a more balanced approach: Identifying genuine allergic conditions, avoiding superfluous needle pricks, and equipping families with effective, practical tools and strategies to manage allergies early and efficiently.
**Pediatric Allergy Landscape**
According to the CDC’s 2021 statistics, 18.9 percent of children in the U.S. have a diagnosed seasonal allergy. Boys (20.0 percent) are slightly more affected than girls (17.7 percent). There are also racial and ethnic disparities: Non-Hispanic Black (21.3 percent) and non-Hispanic White (20.4 percent) children report higher rates than Hispanic (15.3 percent) or non-Hispanic Asian (11.0 percent) children. These variances may be indicative of a combination of genetic factors, environmental exposures (such as indoor allergens and pollution), and inequalities in access to diagnosis and specialty care.
So why not simply test for environmental allergens?
Well, in practice:
– Positive results do not always indicate clinical illness. Children may exhibit IgE positivity levels without symptoms, leading to misleading positive outcomes and increased anxiety.
– False reassurance: Negative tests can lead families to inaction.
– Financial and access challenges: Panels may lack insurance coverage and impose a financial burden on families.
**Identifying Allergies Through Clinical Presentation and Specific Indicators**
Before rushing to testing, a more effective method involves recognizing allergies through comprehensive history and examinations.
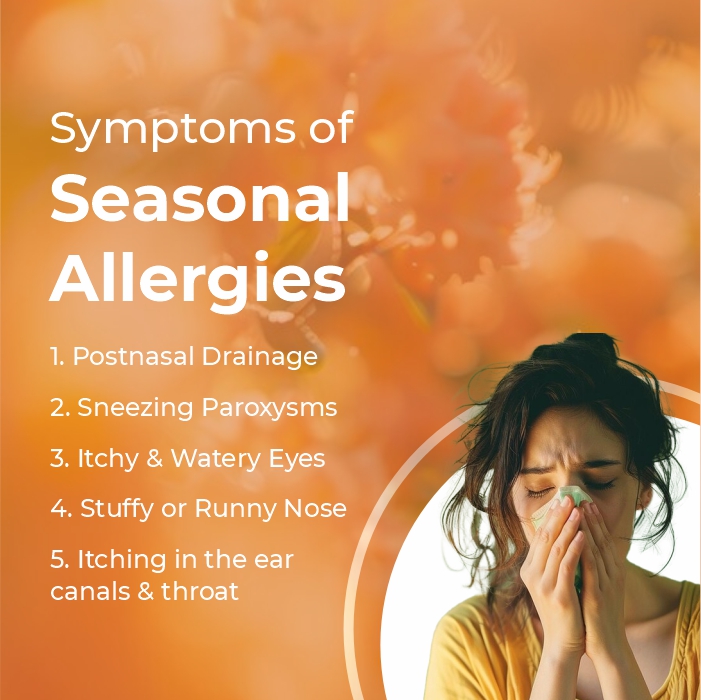
**Symptom trends:**
– Do symptoms recur during the same season annually?
– Are they provoked or exacerbated by pollen seasons, windy, dry days, or known allergen exposures?
– Symptoms such as itchy eyes or nose, sneezing, clear nasal discharge, postnasal drip, and nasal congestion, particularly in the absence of fever.
– Persistence beyond 10-14 days or recurrence across different seasons.
**Any related features:**
– Eczema, asthma, and a family history of allergies.
– Responses to previously prescribed medications (e.g., antihistamines, nasal steroids).
**Physical indicators:**
– Nasal examination: pale or boggy mucosa, cobblestoning of the posterior pharynx, allergic shiners.
– Eyes: dark circles beneath the eyes, itchiness, excessive clear, watery discharge.
**Practical Home-Based First-Line Strategies for Families**
According to AAP’s recommendations, allergen avoidance and symptomatic treatments should be the first steps, with testing reserved for select cases. Some of these measures include:
**Environmental controls and avoidance**
– Keep windows closed on high pollen days.
– Use HEPA filters indoors.
– Wash bedding weekly in hot water.
– Employ allergen-proof covers on mattresses and pillows.
– Maintain indoor humidity below 50 percent.
– Reduce carpet use in bedrooms.
– Pet management: If pets trigger symptoms, consider limiting their access to bedrooms, restricting interactions to specific areas of the home, or housing them in kennels.
– Ensure proper ventilation in bathrooms and kitchens, and routinely check for and eliminate mold in sensitive areas.
– Take a shower before bed, rinse off pollen, and change clothes after being outside.
**Over-the-Counter (OTC) Medications**
– Non-sedating antihistamines for sneezing, itching, and runny nose: Initiate treatment as soon as symptoms appear; consider daily preventive use during peak pollen months.
– Saline nasal spray serves as a safe adjunct, especially for nasal congestion or thick secretions.
These strategies frequently alleviate symptom burden significantly, sometimes rendering testing entirely unnecessary. It’s advisable to consult your child’s pediatrician to weigh risks against benefits.
**When Is Testing Indicated?**
Testing using standard environmental panels proves beneficial only when:
– Symptoms persist despite optimal first-line therapy.
– A child qualifies for monthly allergen immunotherapy.
– Unusual or multiple triggers are suspected.
– There is uncertainty in diagnosis or overlapping conditions.
**What Test to Use When?**
Always opt for targeted testing rather than a broad/”shotgun” panel approach.
– Skin prick testing is recommended for inhalant allergens.
– IgE blood panels may be utilized, particularly if skin testing is impractical, such as in children with uncontrolled asthma or eczema or recent/current usage of OTC medications.