### Bridging the Gap in Opioid Treatment: The Case for Reforming Methadone Access
The opioid crisis is a persistent public health emergency, claiming tens of thousands of lives each year in the U.S. At the forefront of the fight against opioid use disorder (OUD) is the accessibility and efficacy of medications for opioid use disorder (MOUD), including buprenorphine and methadone. Yet, bureaucratic obstacles surrounding methadone, a crucial medication in addressing OUD, hinder many patients from obtaining it. The experience of Kayla, a young woman whose worsening fentanyl use drove her to seek assistance at an addiction clinic, highlights the necessity for reforms like the proposed **Modernizing Opioid Treatment Access Act (MOTAA)**.
—
### **The Promise of MOUD**
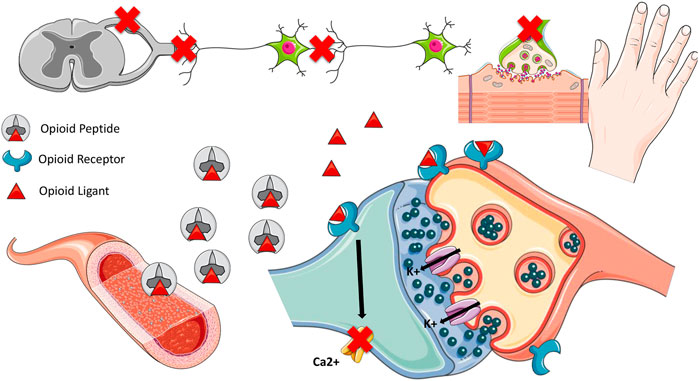
Utilizing MOUD, including buprenorphine and methadone, significantly decreases mortality related to OUD. These medications target opioid receptors in the brain, alleviating the unending cycle of withdrawal and cravings that sustain drug use. Research indicates that initiating treatment with MOUD can lower the risk of death for individuals with OUD by around **50%**. In addition to survival, these therapies restore independence, enabling patients to regain command of their lives and reintegrate into their communities.
For many individuals, buprenorphine, a partial opioid agonist, is the preferred initial therapy due to its safety and availability at local pharmacies. However, the rising prevalence of fentanyl has complicated treatment options. Fentanyl’s remarkable potency establishes tolerance levels so high that buprenorphine may not sufficiently mitigate withdrawal symptoms or cravings. More alarmingly, **transitional errors when moving to buprenorphine** can lead to withdrawal, a situation exacerbated by the potency of synthetic opioids. Consequently, methadone—a full opioid agonist and powerful alternative—has become a critical medication for numerous patients.
—
### **The Methadone Paradox**
Despite being one of the most effective solutions for opioid addiction, a complex set of federal and state regulations significantly limits methadone availability. Methadone for OUD can only be dispensed through **Opioid Treatment Programs (OTPs)**, where patients must visit daily or several times a week to receive their doses under supervision. This approach, established many years ago, unintentionally generates considerable obstacles:
1. **Geographic and Scheduling Challenges**:
Individuals may need to travel considerable distances to access OTPs. Limited operating hours force many to attend early morning dosing, a schedule that conflicts with employment, childcare, or other responsibilities.
2. **Stigma and Fragmented Care**:
Patients like Kayla, who seek assistance from primary care providers or addiction specialists, are unable to obtain methadone from their usual healthcare sources. Instead, they must navigate a separate, often stigmatized healthcare system provided by OTPs.
3. **Disruption of Life Stability**:
Kayla’s apprehension of losing her overnight job due to early morning OTP appointments reveals the disruption caused by the existing methadone dispensing model. For those already in precarious socioeconomic situations, this can be a significant barrier to ongoing treatment.
Ironically, methadone prescribed for pain management is accessible at community pharmacies. This inconsistency in regulation highlights the stigma surrounding addiction and perpetuates outdated methods of treating OUD.
—
### **Lessons From the Pandemic**
The COVID-19 pandemic compelled policymakers and health systems to adjust rapidly. To minimize virus spread and accommodate an unprecedented rise in overdose fatalities, **methadone regulations were relaxed** temporarily. Patients were allowed to receive 14- or 28-day take-home doses, alleviating the financial and logistical pressures of daily clinic attendance. Data gathered during this time showed:
– **Improved patient outcomes:** Enhanced access to methadone did not lead to a significant rise in diversion or overdose incidents, challenging longstanding concerns.
– **Sustained engagement in care:** Freed from stringent clinic schedules, many patients maintained adherence to their treatment protocols.
In light of these advantages, the Department of Health and Human Services formalized these expanded take-home allowances in the “Final Rule,” effective October 2024. However, while this is a positive development, it fails to resolve the fundamental separation of methadone from standard addiction treatment practices or its accessibility within the community.
—
### **How MOTAA Can Transform Care**
The **Modernizing Opioid Treatment Access Act (MOTAA)** aims to take methadone reform further. If enacted, MOTAA would permit addiction specialists to prescribe methadone for OUD, with prescriptions filled at regular community pharmacies rather than OTPs. This would:
1. **Expand Access to Treatment**:
Patients would be able to obtain methadone from their current healthcare providers, integrating OUD treatment into the wider healthcare system. This is particularly crucial in rural or underserved regions where OTPs may not be available.
2. **Reduce Stigma**:
Dispensing methadone through community pharmacies would normalize methadone treatment.