Title: The Disappearing Physician Mentor – An Urgent Challenge Impacting the Complete Healthcare Landscape
By Kenneth Botelho, DMSc, PA-C
The gradual decline of physician mentorship isn’t simply a wistful reflection on the past—it represents a growing crisis with extensive implications for the healthcare ecosystem. While the national attention is focused on physician burnout and workforce deficits, the concurrent vanishing of robust clinical mentorship frameworks—especially in primary care—has received less attention, but remains critically important. A notable group feeling the effects of this transition is the physician associate/assistant (PA) workforce.
Historically grounded in a strong tradition of apprenticeship, PAs were trained under the direct supervision of seasoned physicians. This relationship served as the foundation for both clinical and professional growth, nurturing competence and self-assurance in new clinicians. However, that foundation is now disintegrating.
Physician Retirement Creates a Gap
As the physician demographic ages and numerous primary care physicians move away from clinical responsibilities—whether through retirement, early exits due to burnout, or shifts to nonclinical positions—the apprenticeship paradigm that bolstered many PA trajectories is unraveling. Reports from students and peers reveal that early-stage PAs are often thrust into high-need positions with little oversight and increased productivity demands. The emotional burden is considerable.
As the founding director of a Doctor of Medical Science (DMSc) program and someone closely involved with PA trainees, I consistently hear stories of young professionals in turmoil. These new PAs seek mentorship—not only in clinical decision-making but also in managing ethical challenges, professional relationships, and the emotional burdens inherent to patient care. Pressed for time and resources, many healthcare organizations unwittingly prompt these newcomers to “navigate it themselves.” The fallout includes elevated burnout rates, clinical mistakes, emotional detachment, and workforce turnover.
We Cannot Restore What Has Disappeared—but We Can Rethink Our Future
It is crucial to understand: this isn’t a plea to reconstruct a physician mentorship system that is no longer viable. Pragmatically, we cannot revert to a methodology rooted in a different healthcare context. Nevertheless, this doesn’t imply a lack of options. We possess formidable resources—if we choose to acknowledge and utilize them.
Postgraduate PA educational initiatives—such as fellowships and residencies—provide organized, specialty-oriented avenues for mentorship, skills development, and professional identity formation. These programs are particularly essential in areas like primary care, psychiatry, emergency medicine, and rural health, where the demand is highest. However, these residencies are still limited, underfunded, and undervalued. Numerous health systems view them as indulgences rather than seeing them as vital elements of workforce development.
A Way Forward: Merging Clinical Fellowships and Doctoral-Level Learning
Where do we proceed from this point? I contend that the solution lies in innovation—especially at the crossroads of structured fellowship training and advanced education. Doctor of Medical Science (DMSc) programs, particularly those designed for current PAs, offer a unique opportunity to serve as academic foundations for clinical fellowships. These doctoral programs can integrate postgraduate training within comprehensive curricula that encompass value-based care, leadership skills, medical ethics, and collaborative care—preparing PAs to not only practice proficiently, but also to lead, teach, and advocate for future healthcare providers.
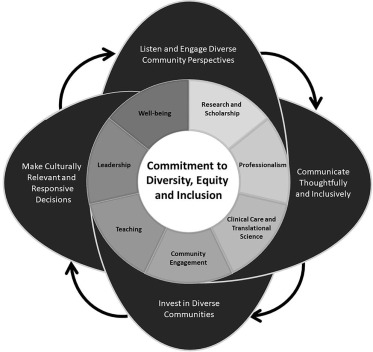
Our team has begun to bridge this divide, transforming fellowship programs to not only improve clinical competencies but also cultivate leadership skills and systemic understanding. As healthcare swiftly transitions towards intricate, multidisciplinary frameworks, we must actively prepare PAs to take on roles previously reserved for physicians—including mentorship functions.
Developing Sustainable Models
For any of this to succeed, however, we need to change our collective perspective. Expanding postgraduate PA education—and appropriately funding it—must be regarded as a strategic, systemic investment. Healthcare systems, educational organizations, and policymakers need to perceive mentorship not merely as a supplementary option but as a fundamental responsibility linked directly to patient care, workforce retention, and ethical oversight.
Let’s be clear: no doctoral program, regardless of how well constructed, can completely substitute the insight and complexity of continuous, direct physician mentorship. However, we can create new solutions that address the system’s current state. These models should be interprofessional, scalable, and reflective of present-day realities. Without such initiatives, the gap will only widen, leaving newer clinicians—frequently thrust into demanding situations before they are ready—to bear an overwhelming burden independently.
The Risks Are Too Great to Postpone
If we neglect to tackle this increasing void, the ramifications extend far beyond the educational sphere. The persistent absence of mentorship jeopardizes both provider well-being and patient safety. It also threatens our capacity to retain talented, committed PAs who are motivated to make a difference in communities where access to care is already limited.
However, if we take decisive action—investing in educational reforms, practice-based training, and interprofessional models—we can redefine mentorship in ways that empower not only learners but also patients as well.