Title: Enhancing Health Care Communication Accessibility for Individuals with Aphasia
In an ordinary health care environment, a patient might describe symptoms while a physician enters notes into a computer. For many, this seems like a standard procedure. However, for those with aphasia—a language impairment that hinders a person’s ability to speak, comprehend, read, or write—this exchange can be incredibly frustrating and isolating. Something as straightforward as a doctor facing away to input data can unintentionally lead to a communication breakdown, particularly when visual cues such as facial expressions, lip movements, and eye contact are crucial for comprehension.
This straightforward yet impactful statement—“There are times when doctors type notes while my back is turned as I communicate. I have aphasia. I need to see people’s mouths and eyes to aid my understanding.”—highlights a larger challenge confronting those with communication disabilities: access.
As a certified speech-language pathologist (SLP) and former sign language interpreter, my experience with individuals who have communication disorders has been extensive. Time and again, I hear tales of frustration from patients who feel marginalized in their own care processes—not due to their cognitive capabilities, but due to the environment and communicative practices employed by health care providers.
The Importance of Effective Communication Access
Communication is fundamental to health care. When it falters, it can not only compromise the quality of care but also jeopardize patient safety. Research shows that individuals with communication disabilities often experience poorer overall health outcomes, including elevated rates of chronic illness, delays in treatment, and increased hospital visits. These inequalities are primarily linked to inaccessible communication during medical appointments.
Real-world repercussions include:
– Medical mistakes stemming from miscommunication
– Incomplete adherence to treatment plans
– Missed diagnoses due to ineffective information exchange
The financial impact is also substantial. A 2018 study featured in Perspectives of the ASHA Special Interest Groups revealed that ineffective communication within U.S. hospitals contributes to approximately $29 billion in preventable adverse events each year.
Time Pressures vs. Human Requirements
Health care providers frequently mention time constraints as impediments to effective communication. The pressure to quickly evaluate, diagnose, and treat is immense. Yet, a few moments of concentrated attention and thoughtful interaction at the beginning of a visit can create significant positive change.
One straightforward question—“What communication supports do you require?”—can proactively set the stage for a more inclusive and effective interaction from the very beginning. By asking this question, accommodations become normalized, recognizing the patient as an essential partner in their health journey.
ASHA’s Communication Access Initiative
To tackle these issues, the American Speech-Language-Hearing Association (ASHA) introduced the Communication Access initiative: “Better Health Starts with Effective Communication.” This initiative promotes health equity by ensuring that every patient can access and comprehend health information in manners that align with their individual needs.
At the core of this initiative is the ACCESS Framework, a six-step strategy for health care professionals:
A – Inquire about communication preferences and requirements prior to care commencement.
C – Directly communicate with the individual, not just at them or through others.
C – Regularly verify comprehension throughout the conversation.
E – Remove distractions, keeping focus on the patient.
S – Slow down to provide adequate time for processing and replies.
S – Facilitate communication using diverse methods (e.g., writing, gestures, visual aids, assistive devices).
These guidelines are not only effective but are often straightforward and affordable to adopt.
The Role of Audiologists and SLPs
Audiologists and SLPs working in clinical, hospital, or outpatient environments play crucial roles in embedding communication access within health care systems. They offer:
– Training for staff on how to engage with patients who have communication disabilities
– Review and modification of patient-facing materials and settings to enhance accessibility
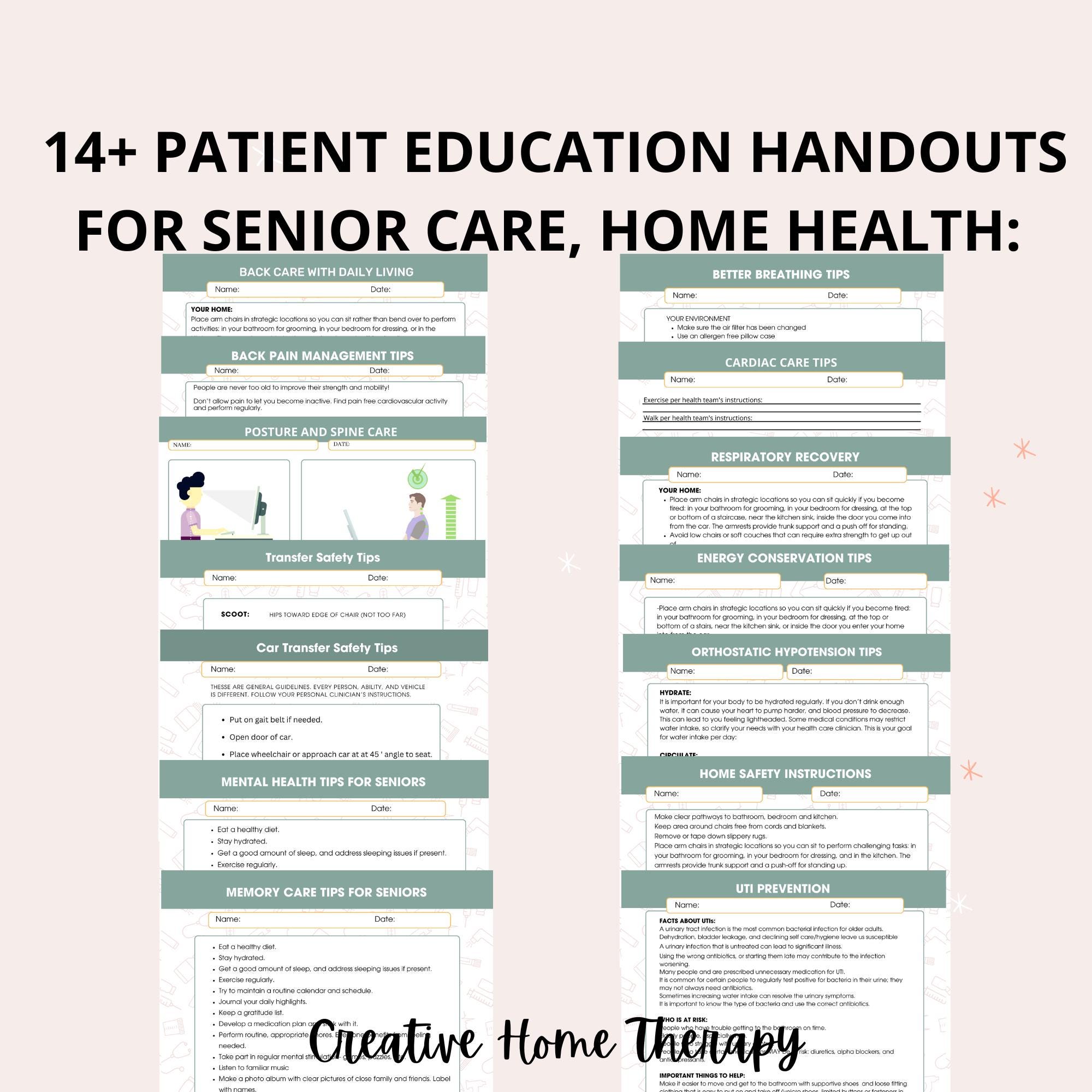
– Strategies for conveying complex information through accessible formats
– Integration of assistive technologies and augmentative and alternative communication (AAC) tools
They also empower patients and their caregivers by:
– Teaching medical terminology and encouraging self-advocacy
– Preparing health records and access plans before appointments
– Customizing communication aids based on individual needs
Creating a Future of Inclusivity
By committing to inclusive, patient-centered communication as a fundamental standard of care, we guarantee that individuals with communication disabilities receive equitable care quality. Being deliberate in our communication enhances not only outcomes for those with aphasia or other communication hurdles but also the overall effectiveness and compassion within the health care system.
By accepting the simple fact that communication is not a one-size-fits-all approach, we progress toward a health care system that genuinely serves everyone.
For additional resources or to connect with communication access experts, consider reaching out to audiologists or speech-language pathologists within your local health system. Learn more about the ASHA Communication Access Initiative at https://www.asha.org/practice/communication-access/.
The next time you encounter a patient who appears to have difficulty expressing themselves or comprehending, don’t turn away. Turn toward them—and create a path not just to care,