Title: Transforming Type 2 Diabetes Management by 2025: Embracing Healing Over Mere Control
By 2025, over 38 million individuals in the United States—approximately 1 in 10—will be navigating the challenges of Type 2 diabetes, presenting a critical public health issue impacting every facet of life, from personal health to the national health expenditure. Historically, the treatment of diabetes has depended on medicinal approaches focused on symptom control rather than addressing the underlying condition. However, a transformative perspective emerging from top endocrinologists, including Dr. William Hsu from Harvard’s Joslin Diabetes Center and L-Nutra, is changing the narrative around Type 2 diabetes—emphasizing remission and long-lasting health rather than just symptom alleviation.
An Inadequate Chronic Disease Framework
Central to the current methodology is a chronic disease framework that frames diabetes as a lifelong issue to be managed rather than possibly overturned. Typically, individuals with Type 2 diabetes are prescribed an average of six different medications to regulate blood sugar levels, insulin resistance, and related health concerns. While this strategy may achieve short-term symptom relief, it often incurs significant physical, emotional, and financial burdens on patients.
This conventional method also seldom tackles the underlying factors contributing to Type 2 diabetes—such as pronounced insulin resistance, compromised pancreatic function, and metabolic disorders stemming from early aging. Without rethinking our approach to these core imbalances, the impact of this condition will persist. The American Diabetes Association has lately acknowledged remission as a legitimate clinical objective, indicating a significant shift towards prioritizing comprehensive healing over mere management.
Towards Lasting Solutions: Nutrition as a Fundamental Approach
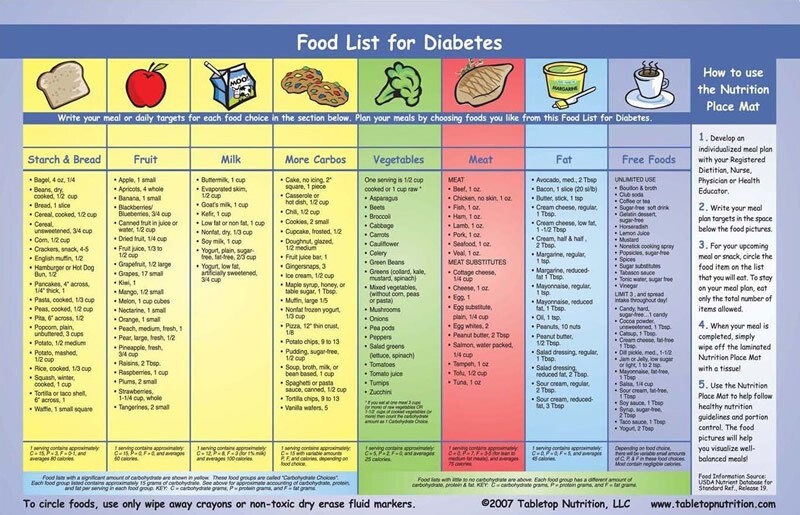
Dr. Hsu and fellow specialists advocate for moving past medication-centered therapies to embrace integrative, nutrition-focused treatment models. This entails shifting away from limited strategies like counting calories and controlling glucose independently, redirecting focus to therapies that target the multifaceted metabolic origins of the ailment.
One promising strategy is the Fasting Mimicking Diet (FMD), a five-day nutritional regimen that replicates the metabolic benefits of fasting. In contrast to certain popular diets such as the ketogenic diet—which may lead to short-term glucose regulation but could result in long-term cardiovascular and cancer-related issues due to high fat and protein consumption—FMD promotes fat burning while safeguarding lean muscle and enhancing overall cellular vitality.
The FMD is intentionally crafted to foster a mild ketosis state without sacrificing vital nutrients. This aids in resetting metabolic pathways, boosting insulin sensitivity, and potentially facilitating the regeneration of pancreatic beta cells, a crucial step towards reversing or even achieving remission from diabetes.
Implementing the FMD in Clinical Settings
A standard FMD program for those with Type 2 diabetes consists of a five-day cycle conducted monthly during the initial six months, then every three months for the subsequent six, all under careful medical and dietary supervision. Throughout these cycles, patients undergo laboratory assessments and have regular consultations with healthcare providers to confirm the diet’s safety, efficacy, and customization to their specific nutritional needs.
After one year, patients are encouraged to continue the five-day FMD two to three times a year, incorporating it into a long-term strategy that promotes longevity and lessens dependence on medications. This well-structured and supportive method offers a far more feasible and lasting intervention compared to daily regimens that demand extreme caloric limitation or strict dietary compliance.
Primary Benefits of FMD-Based Treatment:
1. Metabolic Revitalization: Triggers beneficial fasting-like states without total caloric deprivation, lowering insulin resistance and reducing visceral fat.
2. Muscle Conservation: Promotes fat loss while sustaining muscle mass, critical for metabolic well-being and functionality.
3. Promoting Healthy Aging: Aids in cellular renewal and may delay the onset of age-linked chronic conditions.
4. Long-Term Viability: Designed for periodic application, making adherence easier for patients over time with observable outcomes.
5. Customized Monitoring: Encompasses interdisciplinary care teams that meticulously track advancements and adjust medications as needed.
The Evolution of Diabetes Management Is Imperative
The current treatment paradigm must broaden to encompass remission and regression as feasible targets, highlighting disease progression prevention and metabolic health restoration. Nutritional strategies, when validated through scientific research and executed within a supervised care environment, can serve as robust instruments that transcend mere symptom masking to engender observable, enduring health improvements.
This holistic and restorative philosophy brings optimism—not only for managing diabetes but for revitalizing lives. As emphasized by Dr. Hsu, we must redirect our focus from simply managing chronic illness to conquering it, one patient at a time.
Conclusion
The concerning escalation of Type 2 diabetes occurrences necessitates a courageous reevaluation of our care strategies. Now more than ever, adopting innovative, sustainable, and metabolism-focused approaches like the Fasting Mimicking Diet is not merely advantageous—it is crucial.
By integrating scientific customization, nutritional advancement, and proficient medical supervision, methodologies such as FMD provide not just a temporary solution, but a new horizon in achieving remission, restoring health, and prolonging life expectancy. The healthcare infrastructure must evolve in response to this pressing need.