Title: The Concealed Toll of Procrastination: The Importance of Prompt Specialist Referral in Spinal Surgery
Chronic back pain is a prevalent and progressively burdensome health concern, resulting in countless hours forfeited to discomfort, limitations, and emotional turmoil. Individuals grappling with severe spine issues frequently visit a surgeon’s practice only after suffering for years—sometimes even decades—through conservative treatments such as physical therapy, medication, and injections. While these approaches can be beneficial for many patients, others find themselves in a cycle of stagnation that postpones essential surgical care. Unfortunately, this postponement can lead to irreversible harm, compromised treatment results, and losses in quality of life that could have been prevented.
As a specialist in orthopedic spine care, I advocate for a well-rounded, evidence-based strategy for treating spinal conditions. Conservative options typically stand as sensible first-line treatments. Nonetheless, extended reliance on these methods without progress can ultimately backfire. It’s essential to discern when non-surgical treatments have reached their limit and when surgery should logically follow—timing can swiftly shift from being an ally to becoming an adversary.
The Fallacy of Surgery as the Final Option
A deeply damaging belief among patients—and sometimes perpetuated by healthcare providers—is that spine surgery must be an absolute last resort. This widespread misconception often stems from fears surrounding surgery, outdated medical guidance, or anecdotal horror tales. Although surgery isn’t suitable for everyone, delaying the decision past the ideal intervention timeline can severely diminish the chances of a successful outcome.
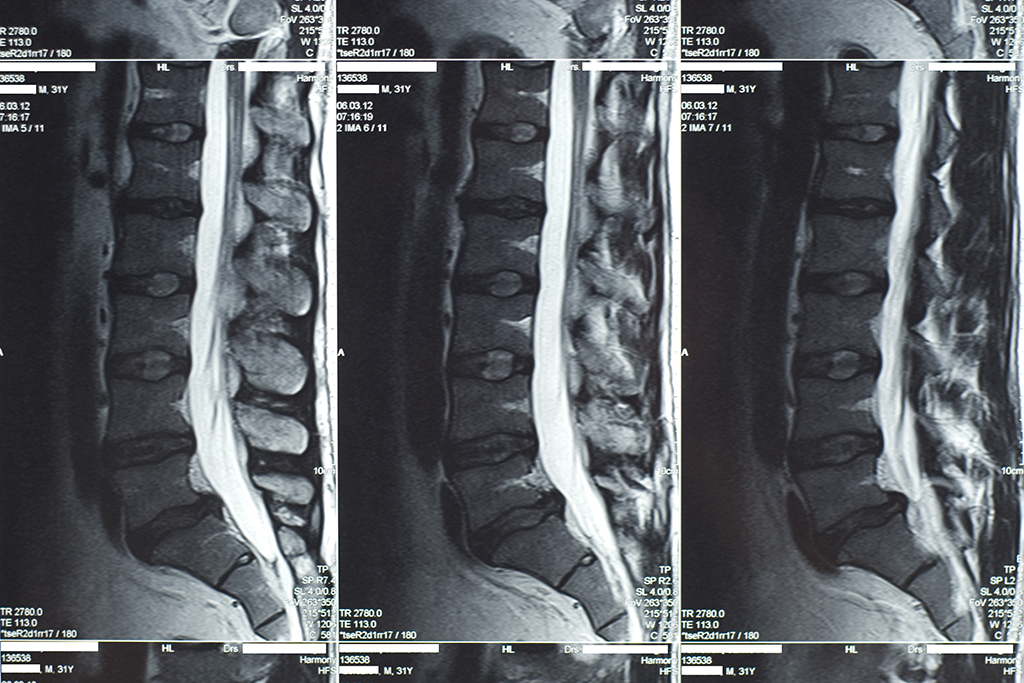
For instance, lumbar disc herniations in their initial stages can typically be effectively treated with a straightforward microdiscectomy, alleviating nerve pressure and restoring function. However, if left untreated, the issue can lead to chronic nerve damage and muscle wasting that become less responsive to surgical solutions. Likewise, untreated spinal stenosis may cause permanent nerve compression, depriving patients not just of movement but also of their autonomy.
The Function of Primary Care Providers
Primary care physicians (PCPs) are at the forefront of identifying and addressing spinal concerns. They play a vital part in navigating patients through their treatment choices and figuring out when referrals to spinal specialists are necessary. Unfortunately, due to unclear referral criteria or a tendency to over-rely on conservative treatments, essential intervention opportunities are often overlooked.
I strongly recommend that once patients experience ongoing symptoms—particularly neurological signs like numbness, tingling, or muscle weakness—for more than three to six months despite conservative therapy, they should be sent to a spine specialist for a thorough assessment. A referral does not guarantee immediate surgery; instead, it provides patients with access to a range of treatment strategies, both surgical and non-surgical, customized to their unique condition.
The Collaborative Framework: A Superior Path Forward
Enhancing outcomes in spinal surgery requires a team-oriented, patient-focused methodology. Collaboration among primary care physicians, physical therapists, pain management specialists, and orthopedic surgeons guarantees that patients receive prompt and suitable interventions. Early diagnosis is crucial, but the ability to act on that information is essential for achieving better results.
When surgery is warranted and executed timely, the outcomes can be remarkably transformative. Patients regain their independence, return to work, and re-engage in daily activities that once appeared unattainable. Procrastinating on surgical care not only prolongs suffering but also heightens the risk of complications, extended recovery periods, and the necessity for more complex interventions later.
Conclusion: Reevaluating the Timeline
Chronic back pain doesn’t always necessitate surgery—but when it does, prompt action can be crucial. Contemporary surgical methods are safer, more precise, and less invasive than ever before. Thus, both patients and healthcare practitioners need to move away from rigid adherence to the “last resort” mindset and toward a more nuanced evaluation framework that considers treatment efficacy, quality of life, and the potential for full recovery.
Ultimately, postponing surgery is not a neutral option—it frequently comes with irreversible repercussions. The cost is not merely measured in pain or inconvenience, but also in long-term disability, lost chances, and avoidable suffering. Empowering patients through education, timely referrals, and well-coordinated care enhances not just individual results but also fortifies the health system at large.
Dr. Gbolahan Okubadejo is a board-certified orthopedic spine surgeon committed to maximizing spinal health through thorough, individualized care. Discover more about him on his LinkedIn profile.