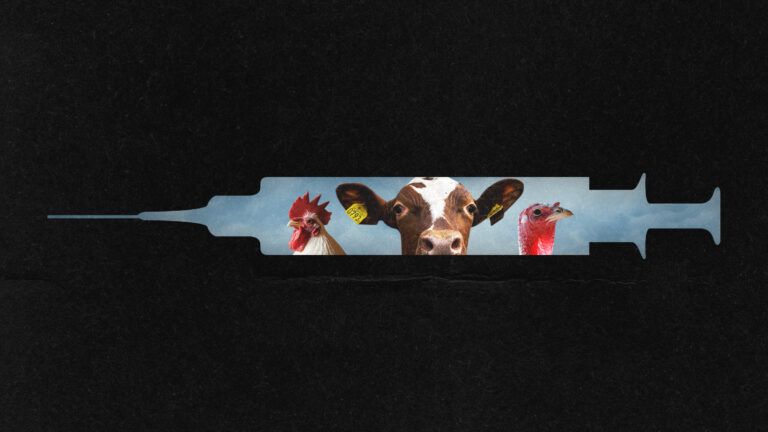
In March 2024, an unforeseen and concerning turn of events emerged in the persistent bird flu (H5N1) saga. Researchers identified the virus breaching typical species barriers and infecting dairy cows in Texas, with the virus found in both the cows and their milk. Following this revelation, the virus began to spread to additional mammals, including goats, domestic cats, dolphins, and humans who came into contact with the infected animals. Although there had been no confirmed cases of human-to-human transmission, the swift cross-species infection raised major alarms.
Throughout 2024, migratory birds played a key role in disseminating the virus across various continents, exacerbating the situation. The U.S. faced widespread poultry outbreaks, leading to significant flock morbidity and mortality, which consequently drove egg prices to unprecedented levels. By early 2025, there were nearly 70 confirmed human cases and one associated death, capturing global attention.
On April 28, 2025, a distinguished group of virologists made a declaration in the Lancet, stressing the importance of enhancing health security measures in response to bird flu. This announcement underscored the critical need for improved testing for both animals and humans, a rise in personal protective equipment for specific professions, expedited vaccine development, and proactive initiatives to mitigate vaccine hesitancy.
Additionally, the year 2025 saw a deterioration of crucial U.S. public health systems, particularly the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA), due to budget reductions. Public health monitoring, akin to milk and wastewater testing initiatives, encountered obstacles. At the same time, vaccine misinformation surged, with a significant percentage of the population struggling to accurately evaluate vaccine-related claims. This culminated in a major measles outbreak, highlighting the numerous challenges experienced during this public health emergency.
The intersection of H5N1’s evolution with institutional and societal trust weaknesses created a volatile scenario, suggesting the potential for a larger pandemic. The need to reassess and revise pandemic preparedness strategies became evident, despite diminishing national and state resources. There was a clear necessity for health professionals to partake in effective public communication and education, utilizing alternative non-governmental channels and social media to combat misinformation. The call for universities, hospitals, and healthcare practitioners to innovate and take the lead in public health education and prevention grew more urgent.
The pressing need is to confront these issues collectively before the next pandemic fully materializes.