Men typically don’t initiate discussions about prostate exams in casual settings, and this reluctance contributes to the issue. In clinics and examination rooms, it’s a common sight: men postponing checkups until urinary problems become troublesome or worse, when routine blood tests raise alarms. The reality is, prostate screening is not about shame or anxiety; it’s about proactively addressing issues that are prevalent, manageable, and potentially serious if neglected.
Let’s explore the details of a prostate exam, when it should be considered, and why it may be one of the crucial steps for your long-term wellness.
**The Importance of Prostate Health**
The prostate is a small gland, approximately the size of a walnut, located just underneath the bladder. As men get older, the prostate tends to enlarge naturally, a condition referred to as benign prostatic hyperplasia (BPH). While it’s not cancer, it can interfere with daily life in annoying ways: a weak urine stream, frequent nighttime bathroom trips, urgency, or struggle with starting and stopping urination.
Even more alarming is prostate cancer, which can grow unnoticed and ranks as the second most prevalent cancer among men globally. In its early phases, it typically presents no symptoms, and by the time symptoms develop, treatment options may be constrained. Regular exams are essential, not to induce stress, but to ensure understanding.
**What to Expect During a Prostate Exam**
For numerous men, the thought of a prostate exam evokes more fear than needed. In actuality, the examination is quick, considerate, and educational.
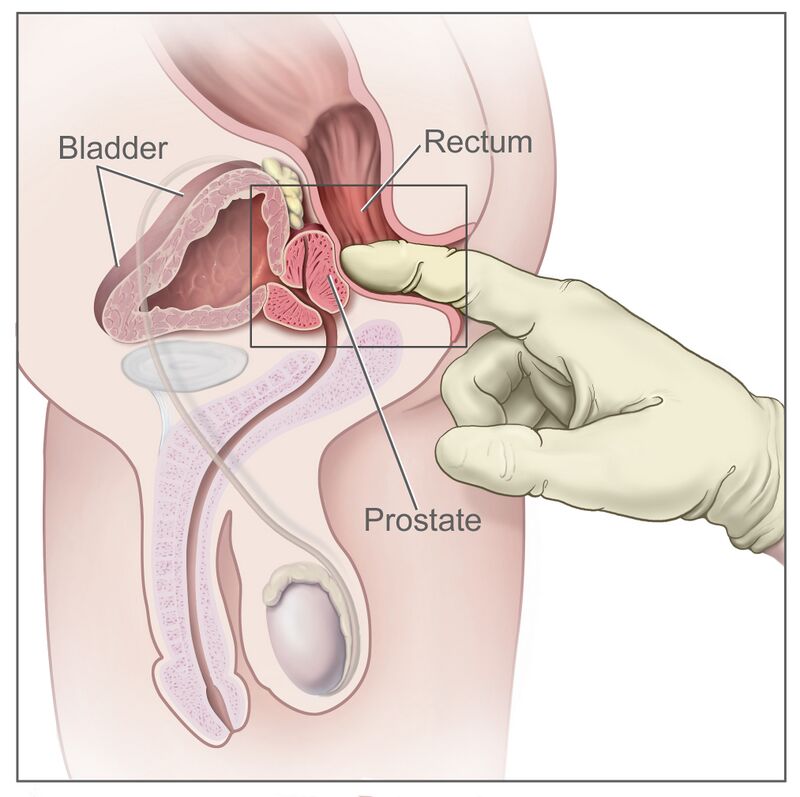
There are two primary parts: the digital rectal exam (DRE) and the prostate-specific antigen (PSA) blood test.
In the DRE, your doctor carefully inserts a gloved, lubricated finger into the rectum to assess the size, shape, and texture of the prostate. This process takes less than 30 seconds and may feel somewhat uncomfortable, yet it is not painful. The PSA test, on the other hand, is a straightforward blood sample that checks for a protein produced by prostate tissue. High levels don’t necessarily indicate cancer; conditions like BPH and inflammation can also elevate PSA, but monitoring changes over time provides important insights. When used together, these methods help detect issues early and determine subsequent actions.
**Reasons for Avoidance**
Numerous men shy away from prostate exams because they believe a lack of symptoms means no issues exist. Others feel embarrassed or fear what the results may uncover. However, avoiding examinations has repercussions.
Early detection of prostate cancer is often very treatable. BPH, if addressed promptly, may not need surgical intervention or even medication. Delaying until symptoms worsen restricts treatment options and can result in unnecessary discomfort, anxiety, or more invasive procedures later. You don’t have to wait for something to feel wrong to take charge of your health.
**What if Abnormalities Are Detected?**
If your PSA levels are high or your DRE raises concerns, your doctor may suggest further evaluation. This doesn’t automatically imply something serious; it merely indicates that more information is necessary. Follow-up could involve repeated PSA testing weeks later, ordering a specialized urine or blood examination, or a referral to a urologist. Depending on your risk factors, imaging techniques like multiparametric MRI may be recommended to examine the prostate more closely. If necessary, a targeted biopsy, often guided by MRI, is conducted to gather tissue samples for examination.
In specific situations, newer genomic tests can assist in assessing the aggressiveness of any identified cancer, aiding in better-informed decisions. It’s essential to understand: most irregular findings are not cancer. But you can’t determine that without investigation.
**When Should You Consult Your Doctor?**
You don’t need to experience symptoms to initiate this conversation. Most major guidelines, including those from the American Urological Association (AUA) and European Association of Urology (EAU), suggest men at average risk should start discussing prostate screening at age 50. If you’re African American or have a first-degree relative (father or brother) diagnosed with prostate cancer, discussing it by age 45 or even earlier in high-risk families is advisable. A simple dialogue with your primary care physician or urologist can help assess if and when screening is appropriate for you.
**Evolution of Screening and Options**
It’s crucial to realize that screening doesn’t automatically result in aggressive treatment. In fact, many early-stage or slow-growing prostate cancers are now monitored through active surveillance, which involves regular observation rather than immediate surgery or radiation. This approach helps prevent overtreatment while still ensuring safety.
Treatment alternatives for BPH and other non-cancerous conditions have significantly expanded over the past ten years. From medications to minimally invasive procedures like UroLift, Rezūm, or HoLEP, the aim is always to enhance the quality of life while reducing side effects and recovery time.
**Concluding Thoughts: Take the Initial Step**
Undergoing a prostate exam isn’t about relinquishing control; it’s about