The night shift was surprisingly tranquil. Mr. T, a 74-year-old admitted due to pneumonia, had finished his evening antibiotics and was resting quietly. His blood pressure, heart rate, temperature, and oxygen saturation readings were all within the normal range. The nurse’s 2 a.m. note was concise yet insightful: “Less communicative tonight,” “Needed prompting to walk to the bathroom,” “Left most of his dinner uneaten.”
By morning, Mr. T had developed a fever, low blood pressure, and confusion. Within hours, he was transferred to the ICU due to septic shock.
Reflecting on this, there had indeed been a shift, but it was not in the vital signs. It was evident in his demeanor, mobility, and interaction with care. These alterations were too subtle to trigger any early warning system based solely on vital signs. They were evident in the notes we compose every day.
**The risks of depending solely on vital signs**
Clinicians frequently rely on a mix of intuition and structured data such as vital signs, laboratory results, and standardized scoring systems as primary indicators of decline. Early warning systems like Modified Early Warning Scores (MEWS) and National Early Warning Score (NEWS2) are beneficial, but they emphasize measurable changes. They may struggle to capture “hesitant to rise from bed,” “slower movements during dressing changes,” or “needing more help to eat.”
In bustling hospital environments, these signs can become obscured by a mountain of daily documentation. Even the most diligent clinician may overlook them, particularly when managing multiple patients or enduring lengthy shifts. The unfortunate reality is that many patients, including Mr. T, begin to exhibit these indicators hours to days before their condition worsens.
**The role of natural language processing (NLP)**
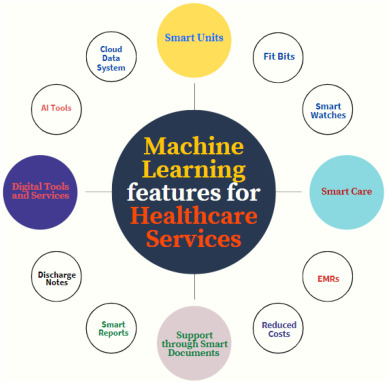
NLP, a subset of artificial intelligence, has the capacity to analyze free-text documentation on a large scale. Instead of merely scanning a handful of recent notes, NLP can process the entire patient chart in seconds, identifying recurring or escalating mentions of significant phrases, even when they are spread across various clinicians’ entries.
For instance, an NLP system might highlight a patient whose last three progress notes reference:
– “Took longer to respond to questions”
– “Required repeated prompting during today’s physical therapy session.”
– “Reluctant to take pills, with increased coughing while drinking water”
On their own, these phrases may appear minor, but collectively, they could signal early delirium, neurological deterioration, or aspiration risks well before any changes in vital signs.
Research has validated the potential of NLP in this field. NLP models can analyze nursing documentation to detect patient deterioration hours to days earlier than vital signs alone. They can recognize patterns in language that describe functional changes closely correlated with adverse outcomes, even among patients who show stable laboratory and vital signs.
Notably, these cues often arise from multiple sources such as doctors, nurses, physical therapists, speech-language pathologists, and even social workers. Humans rarely possess the time or bandwidth to synthesize such extensive documentation in real-time, but NLP can handle this efficiently.
**Considerations for resource-limited environments**
In high-resource hospitals, continuous monitoring, frequent lab assessments, and advanced tracking can help identify deterioration. However, these tools are not widely available in many regions around the globe. What remains prevalent in nearly every inpatient and outpatient environment is solely written documentation.
In these situations, an NLP-driven early warning system could revolutionize care. It would necessitate software capable of extracting insights from the data already being recorded. First, a paper-based chart would need digitization and processing, along with a basic EHR system to run the algorithm in the background. This could significantly improve outcomes where every ICU bed requires high-level resources that are often scarce. In such circumstances, NLP and early intervention can prevent patient decline and the need for intensive care, which, despite best efforts, can sometimes lead to patient loss due to delayed response.
**The significance of meticulous documentation**
NLP functions optimally with the quality of information it receives. Algorithms can misinterpret context. For example, if a nurse notes “patient less talkative,” it is crucial that she also clarifies the context. Was his response appropriate given that it was 2 a.m. and his usual sleeping hours? Was his behavior atypical because he typically wakes up and engages actively at that time, or was his behavior unusual because it was 4 p.m. when he would generally be ambulating and interacting with his peers?
Such careful documentation, paired with other phrases like “less steady,” “more withdrawn,” or “having trouble chewing” over the past twenty-four hours could lead to more precise and timely alerts. Inadequate documentation might result in false alarms.
Another factor to consider is biases present in training data which could also lead to false alarms or overlooked detections, especially for populations that are underrepresented in the data. Transparency, thorough validation, and clinician oversight are crucial.
NLP should be regarded as a supplement to, not a substitute for, clinical judgment. The most effective systems will integrate seamlessly.