Individuals with inherited bleeding disorders, including those with mild to moderate hemophilia and females who are affected, face many challenges that are frequently overlooked in current clinical research and treatment recommendations. Despite improvements in medical care, these individuals continue to have unmet needs that greatly affect their quality of life.
**Unmet Needs**
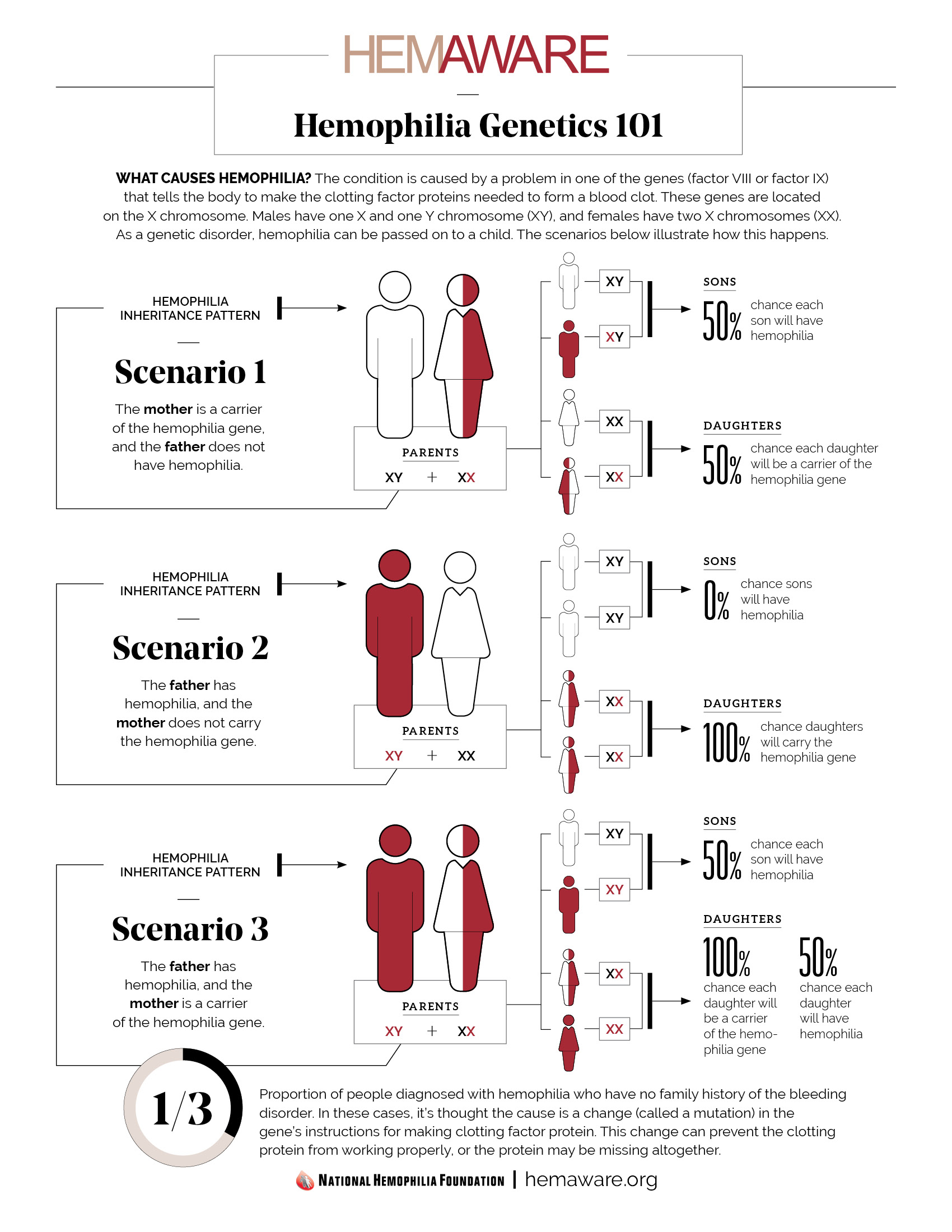
**Diagnosis and Awareness:** Those with mild and moderate hemophilia often suffer from delayed or overlooked diagnoses, leading to untreated bleeding incidents. The belief that hemophilia mainly affects males contributes to underdiagnosis in females, causing their symptoms to be undervalued by healthcare providers and resulting in insufficient care and lowered quality of life.
**Education:** There is a widespread lack of understanding among both patients and healthcare professionals. Many do not recognize the related bleeding risks or the importance of prompt intervention, while clinicians frequently lack insights into hemophilia’s effects on women and individuals with non-severe cases.
**Underdiagnosed and Misclassified:** Women with non-deletional mutations or those classified as carriers may experience symptoms similar to males with mild hemophilia, yet they often receive incorrect diagnoses. The outdated terminology does not accurately reflect their true medical condition. Males are generally diagnosed at an earlier stage, while females with similar symptoms may only receive a diagnosis later in life.
**Lack of Inclusion in Clinical Trials:** Historically, females and individuals with mild to moderate hemophilia have been excluded from clinical trials and registries. This exclusion limits available evidence and restricts the relevance of treatment protocols.
**Absent in Treatment Guidelines:** Prominent hemophilia guidelines mainly address severe cases, overlooking mild cases and females. Women face specific issues, such as menstruation and childbirth, which are seldom considered in existing guidelines.
**Clinical Engagement:** Individuals with mild and moderate conditions, particularly women, often have limited interaction with specialized care facilities and the bleeding disorders community, leading to missed chances for optimal treatment and peer support.
**Quality of Life:** In spite of therapeutic advancements, many still encounter bleeding episodes, joint complications, and challenges in their professional and personal lives.
**Guideline Limitations:** Current recommendations primarily focus on severe cases, leaving those with mild/moderate disorders and females without access to new treatments or prophylactic options.
**Clinical Trial Exclusion:** Individuals with mild/moderate hemophilia and female patients have historically been left out of trials for new therapies, resulting in a lack of direction for optimal management in these demographics and persisting treatment disparities.
**Making the Case for Expanded Access**
**Equity in Care:** To ensure equitable healthcare, there must be an expansion of access to innovative therapies for individuals with mild/moderate hemophilia and females suffering significant effects from bleeding disorders.
**Diagnostic Update:** Contemporary definitions recognize symptomatic females and encompass the full range of disease severity. Treatment should correspond with clinical requirements regardless of traditional classifications or gender.
**Health Outcomes:** Providing appropriate prophylaxis and new therapies to these underrepresented groups can enhance bleeding control, protect joint health, and increase engagement in everyday activities.
**Stakeholder Engagement:** It is essential for guideline committees, regulators, and industry stakeholders to actively involve these populations in trial designs and policy considerations to identify optimal dosing and guarantee efficacy and safety for all affected individuals.
**Education and Advocacy:** Improved education for patients and providers, alongside community programs and focused screening, is crucial to tackle diagnostic shortcomings and enhance access to care.
**Conclusion**
To close the gap in hemophilia care, it is vital to revise diagnostic criteria, educate healthcare professionals, and guarantee the availability of new therapies for underserved populations. Achieving genuine health equity in managing bleeding disorders relies on these initiatives.