A Young Woman’s Experience with Endometriosis and Fertility: An In-Depth Resource
A young woman in her late twenties reached out to me post-surgery for extensive endometriosis. The surgical intervention brought her considerable relief from chronic pain, and her latest follow-up tests showed promising outcomes: her fallopian tubes were open, as indicated by the hysterosalpingogram (HSG), and her anti-Müllerian hormone (AMH) level exceeded 4 ng/mL, which is considered a normal indicator of ovarian reserve. Nevertheless, she had relevant apprehensions: “With my AMH being good and my tubes open, doesn’t this imply all is well? If the doctors are voicing concerns about my fertility, are they merely advocating for treatments?” This inquiry underscores a common misconception in fertility care regarding the actual significance of AMH levels.
Grasping AMH and Its Importance
AMH, a hormone produced by small ovarian follicles, offers insights into a woman’s egg supply, also referred to as her ovarian reserve. An AMH level greater than 4 ng/mL signifies a robust pool of available follicles compared to her peers. However, it is essential to recognize that AMH indicates egg quantity, not quality.
The Fallacy Surrounding AMH
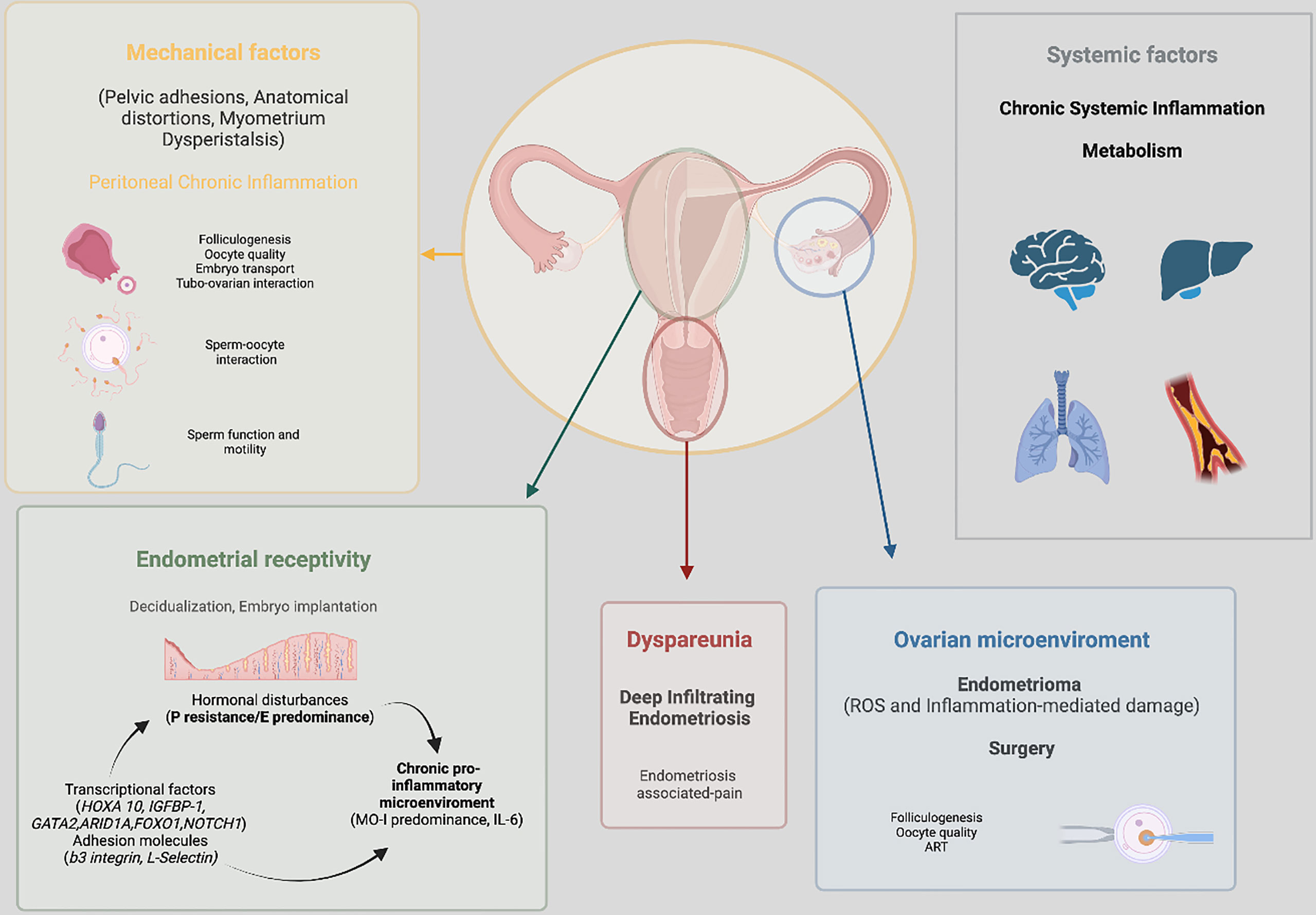
AMH levels by themselves do not dictate egg quality, which is heavily influenced by factors such as age and cellular health, pertaining to elements like chromosomal integrity and mitochondrial function. For instance, a 25-year-old and a 40-year-old might have comparable AMH levels, yet the reproductive capacity of their eggs could differ significantly. In the realm of endometriosis, additional complications can emerge post-surgery. The condition may still affect fertility through:
– Scarring or adhesions that may obstruct the egg retrieval by the fallopian tubes.
– Microscopic inflammation that could influence fertilization, implantation, or embryo development.
Endometriosis and Fertility Obstacles
Research consistently indicates that women with moderate to severe endometriosis experience lower fertility rates than those without the disorder, even if their AMH levels and tube function are normal. Relief from pain following surgery does not equate to restored natural fertility. Recent findings highlight:
– Oocytes from women with endometriosis may exhibit structural alterations that could hinder embryo development.
– The coexistence of endometriosis and adenomyosis has been linked to diminished cumulative live birth rates across various IVF cycles, although many women eventually achieve pregnancy with perseverance.
– Customized treatment strategies, which include tailored stimulation protocols, lifestyle modifications to mitigate inflammation, and possibly additional surgery, can enhance fertility outcomes.
Tackling Fertility Treatment Concerns
Patients often feel pressured when healthcare providers raise fertility issues, but expressed caution is not synonymous with fear-mongering; it is grounded in scientific evidence. Women with endometriosis are not invariably rushed into treatments such as IVF. For a woman in her twenties, with a healthy ovarian reserve and no current discomfort, trying to conceive naturally for six to twelve months could be a reasonable strategy. However, being knowledgeable about the potential fertility implications of endometriosis ensures that critical time isn’t wasted if conception does not occur naturally.
Patient Recommendations
1. While an AMH level above 4 is favorable, it does not ensure superior egg quality.
2. Endometriosis can diminish natural fertility chances even post-surgery.
3. Advanced treatments like IUI or IVF are legitimate options based on individual circumstances—not just alarmist tactics.
4. Partnering with a healthcare provider to formulate a personalized plan that considers age, AMH levels, severity of the condition, and personal fertility ambitions is essential.
Final Thoughts
Endometriosis is complex, and fertility cannot be reduced to a singular test outcome. While certain values are significant, the larger context is equally important. For patients, the focus should be on not dismissing medical advice as intimidation but rather on seeking comprehension, asking questions, and collaborating with a physician who can translate scientific data into a personalized plan for the future.