For more than forty years, I committed my career to surgery, specializing in both general and vascular practices. Nevertheless, the past ten years, characterized by an RVU-based pay structure, represented a pivotal moment in my connection with the medical field. The emphasis transitioned to productivity metrics, trivializing complex, life-saving surgeries to simple numerical values. This unending pressure cultivated a profound sense of dissatisfaction.
In contrast to primary care doctors, surgeons are bound to hospital systems, as major surgical procedures necessitate facilities they govern, rendering us vulnerable to hospital administrators’ decisions. However, a frequently ignored burden is the constant fear of lawsuits.
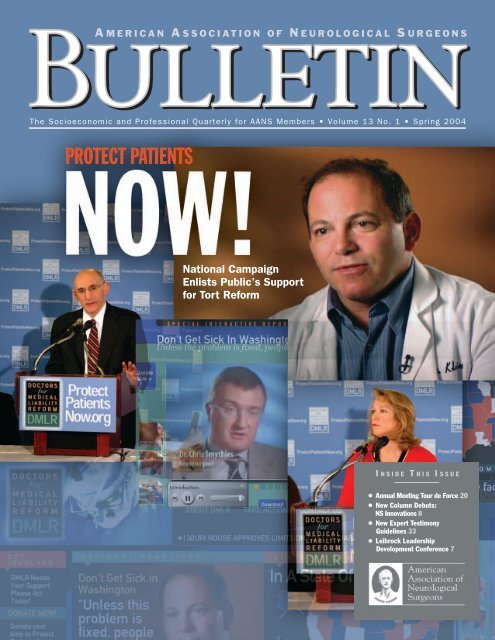
The misconception endures that only negligent physicians face legal action, yet this is a misconception. Legal experts recognize that malpractice insurers often prefer to settle rather than fight in numerous situations. Any case with potential financial benefit results in blanket lawsuits against all physicians involved, regardless of their actual participation. Even a tangential connection carries a stigma, permanently tainting a physician’s record despite the frivolous nature of some claims. Insurers may handle the financial burden, but the psychological and professional fallout rests solely on us.
When I transitioned to wound care, HBOT, and aesthetic medicine, I initially operated under a simple salary framework, appropriate for the variable patient volume and complexities involved. However, during contract renegotiations, a return to the RVU model was proposed. Drawing from my surgical background, I recognized the adverse effects of RVU on wound care—a specialty not characterized by high volume or routine tasks but rather intricate, life-saving efforts—and I declined. My refusal led to contract termination without negotiation, dismissing my considerable experience.
This situation surpasses the concept of burnout—a term simplified to excessive work or inadequate personal time. Authentic burnout arises from a lack of agency. A flawed financial measure dictating income, termination due to an unfair contract disagreement, and unwarranted lawsuits leave a mark of ethical injury.
The pathway after leaving the operating room is markedly constricted. Opportunities to escape hospital dominance do not easily arise, and while stepping back from surgery further restricts options, I remain enthusiastic about contributing through avenues like continued wound care, HBOT, engaging in aesthetics, and exploring fields such as locum tenens, consulting, cannabis medicine, and patient advocacy.
Physicians must candidly address these issues:
– RVUs fail to accurately gauge complex care.
– Contract negotiations should involve discussions rather than ultimatums.
– Malpractice reform needs to focus on tackling unjust lawsuits and their repercussions on wrongly accused physicians.
Advocacy organizations like Take Medicine Back, Physicians Advocacy Institute, and physician unions are starting initiatives but require more support. By sharing my narrative, I hope to shield others from experiencing similar professional sidelining or being overwhelmed by groundless lawsuits.
Despite systemic difficulties, physicians demonstrate a fundamental resilience. Reshaped by the system but not defeated, we can continue to utilize our expertise in environments where healing, advocacy, and contributions endure with dignity.