In a remarkable advancement in the realm of medicine, an individual with type 1 diabetes has commenced generating his own insulin by utilizing genetically modified donor islet cells. A team of researchers in Sweden, spearheaded by Dr. Per-Ola Carlsson, accomplished this by equipping the new cells with an “invisibility cloak,” enabling them to avoid detection by the immune system. This single-patient proof-of-concept investigation, published in the New England Journal of Medicine, brings hope to millions affected by type 1 diabetes.
**The Treatment**
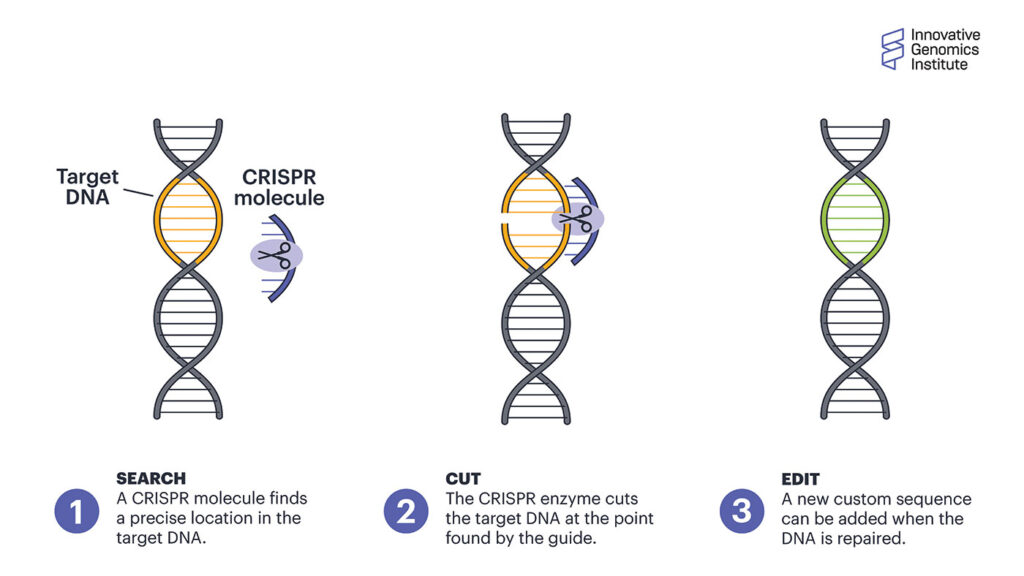
The research group applied CRISPR technology to alter insulin-secreting islet cells from a donor. They disabled two genes, B2M and CIITA, which are responsible for signaling the immune system, and integrated the CD47 gene, recognized as the “don’t eat me” protein. This strategy shields islet cells from immune system attacks. About 80 million gene-modified cells were injected into the forearm of a 42-year-old man who has had type 1 diabetes since childhood. Notably, he did not require any anti-inflammatory or immunosuppressive medications throughout the trial. Researchers tracked his progress for 12 weeks using diagnostic imaging and diabetes management markers.
**What Transpired?**
The researchers evaluated insulin production by assessing C-peptide, an insulin byproduct. The findings revealed that the transplanted cells endured and operated without triggering an immune rejection. C-peptide levels, which were initially undetectable, increased and stabilized over the 12-week period, signifying consistent insulin production. The gene-edited cells were accepted by the immune system, with tenderness at the injection site being the only side effect reported. The patient’s hemoglobin A1C levels decreased by 42%, and he displayed a normal glucose and insulin response to a food challenge.
**What’s Ahead?**
Although the outcomes are encouraging, the case report pertains to just one patient. Additional clinical trials are essential to confirm safety and effectiveness in larger, more diverse populations. The initial dosage was merely 7% of what an adult with type 1 diabetes generally requires, indicating that subsequent trials will increase the dosage and prolong the observation period for long-term safety assessment.
**More Good News from the Other Side of the Globe**
Concurrent investigations at Peking University converted stem cells derived from a 25-year-old woman’s adipose tissue into functional islet cells that produced insulin without triggering an immune response. In just 2.5 months, this patient became insulin-independent and maintained that status for over a year. Although both methodologies necessitate further validation, they represent hopeful pathways toward a potential cure for type 1 diabetes.
In conclusion, this breakthrough, along with other technological developments, heralds a promising future for individuals managing type 1 diabetes, suggesting that a cure may be on the horizon.