In the early stages of the COVID-19 pandemic, healthcare systems rapidly adapted to meet urgent requirements, which included the utilization of yellow fabric isolation gowns. Although these gowns were regarded as a more eco-friendly option in comparison to their paper counterparts, they came with distinct challenges. A frequent problem encountered by healthcare professionals was the ongoing knotting of the neck strings after laundering, leading to discomfort and annoyance, especially for shorter individuals.
This account reveals deeper issues within healthcare infrastructures that were intensified by outside financial pressures. The author shares their experience as a nephrologist and primary care physician at first, eventually moving into the realm of academic medicine. As financial circumstances evolved, the independent community teaching hospital where they were employed was acquired, resulting in the discontinuation of the residency program—a move indicative of larger trends in the healthcare industry.
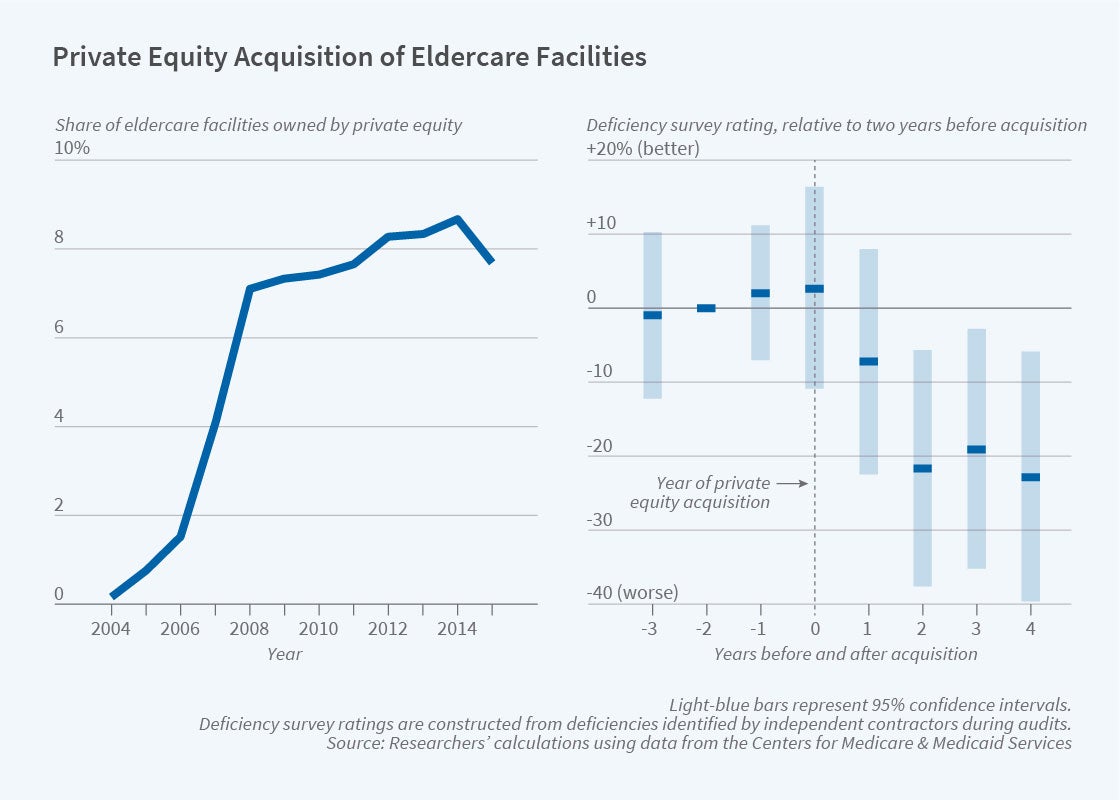
They transitioned to another local hospital, only to face similar financial instability as it was taken over by a private equity-backed firm. Private equity, which prioritizes short-term profit, often clashes with the long-term goals of medical education and patient care. The narrative illustrates how economic uncertainty affects community hospitals, drawing a parallel to the well-known declines of companies like Toys-“R”-Us.
Amid these transformations, healthcare professionals found themselves ensnared in a complicated network of ownership changes and financial hardship, leading to uncertainty and challenges for both staff and patients. In spite of these trials, a spirit of resilience and commitment to medical education endured, allowing the faculty to uphold the residency program and support its trainees.
As the author contemplated their career and the appropriate timing for retirement, recurring themes of dedication to teaching and patient care surfaced. The choice to retire aligned with a reflective view on the growth of residents from novice interns to proficient physicians, highlighting the lasting satisfaction derived from medical instruction.
In the end, the narrative encapsulates not only the personal struggles and experiences of healthcare workers but also the overarching systemic challenges affecting healthcare education and delivery in financially precarious settings. It stresses the necessity of support, resilience, and the quest for education as crucial elements in maneuvering through the intricacies of contemporary healthcare systems.