**U.S. Health Care: A System in Distress**
The U.S. health care model, once celebrated for its creativity and excellence, has devolved into a maze of shortcomings and dissatisfaction. For many individuals, it resembles less of a system and more of a chaotic entity incapable of fulfilling patient needs. As profits for hospitals, pharmaceutical firms, and others in the sector soar, the standard of care diminishes, leaving both patients and doctors frustrated and inadequately served.
### A Personal Experience
As a retired doctor now experiencing the health care system as a patient and caregiver, I have observed its deterioration firsthand. My wife, who faces severe health issues, suffers from excessive wait times, apathetic reactions from medical providers, and a lack of access to urgent services. Our experiences underscore systemic inadequacies, such as a deficit of primary care doctors, which necessitates reliance on nurse practitioners (NPs) and other non-physicians for rapid care.
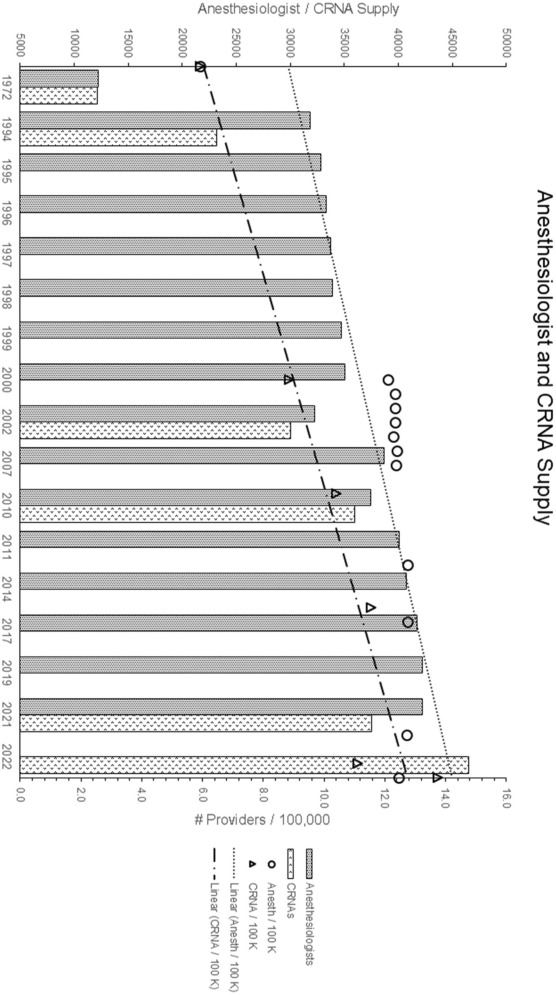
### The Shift to Non-Physician Providers
The growing scarcity of doctors is driving patients toward NPs and other non-physician practitioners. These providers, often more reachable, are addressing the void in primary care—a trend expected to persist with the projected shortage of tens of thousands of doctors in the years ahead. This transition prompts inquiries regarding the future limits of practice and the possible effects on care quality.
### Profits Over Patients
Health care in the U.S. has evolved into a lucratively profitable enterprise. For-profit hospitals, along with certain non-profits, place financial interests ahead of patient care. Bulky administrative structures and private equity acquisitions worsen this dilemma, leading to heightened costs and reduced quality. Such changes divert billions into shareholders’ hands instead of enhancing patient results.
### The Influence of Pharmaceuticals
Pharmaceutical companies have a crucial role in this troubled environment, with medication prices skyrocketing. While promising advancements exist, affordable therapies are frequently disregarded if they don’t align with the profit aspirations of the industry, leaving numerous patients without access to essential drugs.
### Seeking Solutions
Confronting these significant challenges remains complex without clear remedies. Suggestions like broadening medical education, boosting residency opportunities, and incorporating non-physician providers into the care framework are under consideration. However, temporary fixes such as “MinuteClinics” and self-care kits carry their own limitations and dangers.
### The Promise and Risks of Technology
Innovations like telemedicine and artificial intelligence (AI) offer potential improvements for access and diagnostics. Nevertheless, these tools cannot substitute for the vital human aspects of compassion and personalized care that patients depend on.
### Conclusion
The current condition of U.S. health care calls for immediate scrutiny and enhancement. Lives hinge on addressing these systemic challenges, ensuring that care is not merely lucrative but also effective, empathetic, and attainable. As a society and as a profession, we must aim for better health and wellness for our citizens.
*John C. Hagan III, MD, is an ophthalmologist.*