**The Psychotropic Effects of GLP-1 Medications: A Psychiatrist’s Perspective**
In recent times, GLP-1 agonists like Ozempic, Wegovy, Mounjaro, and Zepbound have transformed metabolic health, providing notable advantages in weight control and minimizing cardiovascular risks. Originally intended for diabetes management, these medications have evolved into essential aids for individuals struggling with obesity and its associated comorbidities. Nonetheless, as their usage expands, it is vital to investigate their wider implications, particularly regarding mental health and personality.
**The Parallels with SSRIs**
The widespread emergence of GLP-1 medications brings to mind another significant pharmacological development: SSRIs, such as fluoxetine. Initially praised for their capacity to relieve symptoms of depression and anxiety, SSRIs later became associated with side effects like emotional numbing, reduced libido, and lower motivation. These outcomes emerged as the field refined its comprehension of these medications’ long-term effects on patients’ emotional and psychological well-being.
**The Emerging Pattern with GLP-1s**
As a psychiatrist, the ascent of GLP-1s raises a comparable cautionary narrative. While weight reduction and enhanced metabolic measurements are clear results, a growing number of patients report subtle shifts in personality and affect, particularly at elevated doses. Descriptions of feeling “less alive,” coupled with lowered spontaneity and enthusiasm, align with accounts of muscle atrophy and exhaustion. These physical manifestations can intensify the sentiment of diminished vitality, complicating their emotional experiences further.
**Concerns in Young Patients with Eating Disorders**
Another issue is observed among younger patients, notably those with eating disorders. Many discover comfort in these medications, mentioning a newfound quieting of the persistent “food noise” that often prevails in their minds. However, the suppression of these thoughts may obscure deeper psychological challenges, possibly reinforcing maladaptive coping strategies.
**A Broader Application Yet Limited Data**
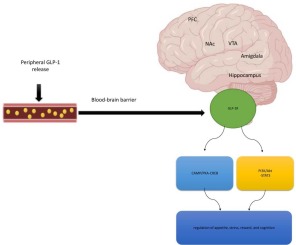
Some healthcare professionals have started investigating the off-label application of GLP-1s for issues beyond diabetes and obesity management, including addictions and mood disorders. While the reduction of cravings can offer potential advantages, the ramifications of curtailing the overall spectrum of desire and motivation present risks that are yet to be fully elucidated through psychiatric inquiry.
**The Need for a Balanced Approach**
The central concern persists that GLP-1s are not just neutral, physical interventions. Recognizing their psychotropic characteristics necessitates a comprehensive approach in their administration. It is crucial to observe not only the numerical achievements, such as weight reduction and blood sugar levels, but also emotional and psychological indicators of well-being, including motivation, happiness, and sociability.
As providers of healthcare, our duty extends beyond immediate physical results. The insights gained from the SSRI era highlight the necessity of tempering initial enthusiasm with ongoing, transparent evaluations of long-term effects. GLP-1 medications stand as a powerful addition to our therapeutic toolkit. However, their application must be directed by holistic care, an understanding of the connection between body and mind, and a steadfast dedication to the overall health of the individual.